-
- Antidepressant Medication
- Baby Partners
- CAHPS Resources
- Care Guidelines
- Developmental Screenings and Surveillance
- Diabetes Prevention Programs
- Disease and Medication Management
- EPSDT / Bright Futures
- ICD-10 Coding and Risk Adjustment
- Lead Screening
- Medication Management and Adherence
- Member Rewards
- Oral Health Resources
- Patient Management
- Patient Safety Reporting
- Quality and Population Health
- Smoking Cessation
- TiPS: Telephonic Psychiatric Consultation Service Program
- Opioid Use Resources

Check this page for important updates on our policies and procedures, announcements, health-related news, our quarterly newsletter and more.

July 7, 2025 - A Practical Guide to Attention-Deficit/Hyperactivity Disorder
Join us for an informative webinar hosted by Jefferson Health on Wednesday, August 6, 2025, where our subject matter experts will provide valuable insights into ADHD. This session will explore the latest understanding of ADHD as a disorder characterized by persistent patterns of inattention, hyperactivity and impulse control.
The webinar will cover topics including:
· Epidemiology and Definitions of ADHD
· Diagnostic Criteria and Screening
· Executive Function and ADHD
· Management and Treatment Approaches
This webinar is ideal for healthcare professionals involved in the diagnosis, treatment, and management of ADHD, including:
· Pediatric Healthcare Providers
· Behavioral Health Specialists
· Primary Care Providers (PCPs)
· Specialists involved in the treatment of ADHD
REGISTRATION DETAILS
Webinars are free, but registration is required. Register now at hpplans.com/webinars.
If you have any questions, call the Provider Services Helpline at 1-888-991-9023 (Monday–Friday, 9 a.m. to 5:30 p.m.) or email providereducation@jeffersonhealthplans.com.
July 2, 2025 - Laboratory Services Reminder
This letter is a reminder to all network providers that all NON-STAT outpatient laboratory services are provided through our vendor, Quest Diagnostics, and hospital locations contracted for laboratory services.
Providers may be reimbursed for STAT lab services performed in the office when the member has a benefit for those services, the provider is contracted to perform those services, and when billed according to policy.
Locations of participating labs can be found via our provider directory.
Please visit our website for the STAT lab payment policy.
If you have any questions or would like more information on how to navigate our provider directory, please contact our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.).
July 2, 2025 - CMS Exclusions Claims Review
In accordance with correct coding guidelines, certain ICD-10 codes cannot be billed together on the same inpatient claim, which could ultimately affect the assigned DRG and associated claim payment.
Effective August 1, 2025, we will be conducting retrospective inpatient claim review. If inappropriate ICD-10 code combinations are identified, the claim will be reprocessed to the appropriate DRG based upon the ICD-10 coding guidance. This could result in a payment adjustment. You will be notified via letter of the impacted claims and related findings as part of this review process.
Please note that medical records and itemized bills will not be requested as part of this review process. The focus is the appropriateness of the billed ICD-10 codes.
If you have any questions, please contact the Provider Services Helpline at 1-888-991-9023.
June 30, 2025 - Home Health Billing Requirements Update
As part of our ongoing commitment to accuracy and efficiency of claim payments, and our concerns over an increased volume of billing errors, effective September 1, 2025, all Electronic Visit Verification (EVV) claims billed by Home Health/Shift Care providers for Health Partners Plans Medicaid members must be billed through HHAeXchange.
EVV claims directly submitted to Health Partners Plans Medicaid will be rejected, which will cause delays in claims processing and payments. As a reminder, we partnered with HHAeXchange in 2021 to provide a free EVV and billing tool for member placement, scheduling, authorization management, communication, and EVV compliance for home health aide services.
Vist www.hhaexchange.com to submit claims and for additional resources. If you have any questions, please contact the Provider Services Helpline at at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
June 25, 2025 - Notification Regarding Independence Day Holiday Hours
In observance of Independence Day, our offices will be closed on Friday, July 4, 2025. We will resume normal business hours on the following business day.
- Claim Payment Cycle – Business as usual for claim payment cycle.
- Provider Helpline - Member eligibility/benefits as well as claim status inquiries can be accessed using the HealthTrio provider portal at hpplans.com/provider-portal.
- Pharmacy Call Center - All pharmacy calls will be forwarded to an outside service center with 24-hour access to an on-call pharmacist by contacting 1-866-841-7659.
- Claims Reconsideration Call Center - Claims reconsideration requests can be submitted through the HealthTrio provider portal at hpplans.com/provider-portal.
- Utilization Management Call Center – On-call services are available at 1-866-500-4571. Authorization requests may be submitted through the HealthTrio provider portal at hpplans.com/provider-portal.
- Enhanced Member Supports Unit Hotline – Members who contact the Enhanced Member Supports Unit will be prompted to leave a voicemail and will receive a return call on the next business day. All messages will be returned on the next business day. The unit may be reached at 1-866-500-4571 (select option 2, then option 7).
As always, we thank you for your continuing efforts to improve the health outcomes of our members.
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
June 20, 2025 - Zelis Itemized Bill Review
Effective June 15, 2025, we are partnering with Zelis to conduct inpatient prospective and retrospective hospital bill reviews on claims which will include requests for itemized bills and/or medical records to verify charges billed.
- Itemized Bill Review – Detailed review of itemized bills to identify billing and coding discrepancies. Errors identified include duplicate charges, unbundling, incidental supplies, and much more.
- Clinical Chart Review – Robust reviews conducted by Certified Coders and/or Clinicians to identify billing, clinical, and coding discrepancies.
These detailed reviews will be conducted by Certified Coders to identify billing and coding discrepancies; errors identified include, but are not limited to, duplicate charges, unbundling, incidental supplies. Identified errors will result in the reprocessing of the claim to adjust the charge amount to align with the review findings. This could result in a payment adjustment.
If you receive a request for review from Zelis, please ensure you follow the instructions outlined in the letter, which also includes contact information directly to Zelis. If you have additional questions, please contact our Provider Services Helpline at 1-888-991-9023.
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
June 19, 2025 - Change to Medication Benefit Limits for Health Partners Plans Medicaid and CHIP Members
Effective June 1, 2025, the benefit limit for some medications will be changing from a 90-day supply maximum to a 30-day supply maximum. This change is effective for the Health Partners Plans Medicaid and Health Partners Plans CHIP lines of business.
The affected drugs are listed below. Please note that these drugs may require Prior Authorization.
Medication Class |
Affected Medications |
New Limit |
||
Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists |
Bydureon Byetta Liraglutide Ozempic |
Rybelsus Trulicity Victoza |
Maximum 30-day supply per fill |
|
Glucagon-Like Peptide-1 (GLP-1) Receptor Agonist/Insulin Combinations |
Soliqua Xultophy |
|||
Calcitonin Gene Related Peptides (CGRP) |
Aimovig Emgality |
|||
For the most up-to-date information regarding Health Partners Plans’ formularies, please visit our formularies page at hpplans.com/formularies. For more information, call our Pharmacy department at 215-991-4300 or our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 4:30 p.m.).
Thank you for your cooperation in improving the quality of care you deliver to your patients and our members.
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
June 17, 2025 - Health Partners Medicaid- PDL Changes to Glucose Meters and Test Strips
This news item is to inform you of upcoming changes to the Pennsylvania Statewide Preferred Drug List (PDL) affecting Health Partners Plans Medicaid.
Below is a list of the changes. These changes will go into effect on July 7, 2025.
Here are the products that are changing to non-preferred status:
Ascensia Glucometers
Contour, Contour Next, Contour Next EZ, Contour Next Gen, Contour Next One, Contour Plus Blue
Ascensia Test Strips
Contour, Contour Next, Contour Plus
Lifescan Glucometers
OneTouch Ultra2, OneTouch Verio Flex, OneTouch Verio Reflect
Lifescan Test Strips
OneTouch Ultra, OneTouch Verio
Here are the preferred alternatives available:
Accu-Chek Glucometers
Accu-Chek Guide
Accu-Chek Test Strips
Accu-Chek Guide
Trividia Glucometers
True Metrix
True Metrix Air
Relion True Metrix Air
Trividia Test Strips
True Metrix
Relion True Metrix
For the most up-to-date information regarding Health Partners Plans formularies, please visit our online formulary at www.hpplans.com/formularies. For more information, call Health Partners Plans’ Pharmacy department at 215-991-4300 or our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.).
Thank you for your cooperation in improving the quality of care you deliver to your patients and our members.
June 6, 2025 - Annual Training for Network Providers Webinar
We are hosting our second Annual Training for Network Providers Webinar of the year on Wednesday, June 11, 2025. All participating providers are required to demonstrate that they are knowledgeable and trained on important topics and participate in at least one webinar each year, offered on a quarterly basis. Participation in this webinar satisfies this annual requirement.
If you are newly contracted with our plan and would like a more comprehensive orientation, please contact us at providereducation@jeffersonhealthplans.com
Topics Include:
- 2025 Updates
- Member Identification Cards
- Prior Authorization Information
- Online Tools (includes portal, website, etc.)
- Credentialing
- Clinical Programs
- Access and Availability standards
- Pay-for Performance and Quality Care Plus
- EPSDT Standards
To register for this and future webinars, visit HealthPartnersPlans.com/webinars, select the webinar you are interested in attending and click the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
ALTERNATE OPTION
While participation in this live webinar will satisfy your annual Jefferson Health Plans’ training requirement, there is an alternative method to complete the training. Please visit https://hpplans.com/provider-online-courses to access the Annual Training for Network Providers (ATP) eLearning course.
June 3, 2025 - Care Coordination Support for You and Your Patients Webinar
We’d like to invite you to an upcoming webinar, Care Coordination Support for You and Your Patients. Our clinical programs can support your practice and your Health Partners Plans Medicaid and Health Partners Plans CHIP patients. These programs help drive Healthcare Effectiveness Data and Information Sets (HEDIS) in a positive direction, which ties to your Quality Care Plus (QCP) reimbursement and overall quality of care you provide.
This webinar will provide a comprehensive look at our clinical programs and resources, including:
- Clinical Connections, which conducts appropriate patient follow-up following a health risk assessment and after a hospital discharge to ensure a patient’s safe transition to their home.
- Baby Partners, which offers coordination of care for pregnant members throughout pregnancy and up to 1 year after delivery.
- Pediatric Care Coordination for children up to age 21, which provides reminders for parents and guardians to ensure patients receive appropriate screenings with guidance from the EPSDT/Bright Future requirements, including help for children with high lead levels, high risk asthma, developmental delays, NICU graduates and children with complex needs.
- Adult Care Coordination for patients (age 21 and older) with a disability or chronic condition.
Webinar Registration Details
The free webinar is on June 18, from 12:30 p.m. to 1:00 p.m. Register now at healthpartnersplans.com/webinars.
If you have questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.) or email providereducation@jeffersonhealthplans.com.
We look forward to your participation and your continued commitment to remain up to date on our resources and programs.
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
June 3, 2025 - Kirby Memorial Health Center Partnership
Lead screening in children is an important preventive measure. Children must have at least one capillary or venous blood test on or before their second birthday.
Effective April 21, 2025, we have partnered with Kirby Memorial Health Center to process lead screenings for Health Partners Plans Medicaid and Health Partners Plans CHIP members. Kirby Memorial Health Center Laboratory is a fully equipped, state-of-the-art laboratory that provides blood lead testing for many Early and Periodic Screening, Diagnostic and Treatment (EPSDT) programs throughout Pennsylvania.
Kirby Memorial Health Center has performed blood lead testing for EPSDT screening programs for over 40 years. The laboratory is certified for blood lead testing by the Pennsylvania Department of Health and CLIA.
A variety of collection supplies are available through Kirby Memorial Health Center for capillector specimen collection. Order forms for supplies are available at www.kirbyhealthcenter.org/clinical-laboratory.
If you need screening supplies or have questions relating to your current supplies and collection method, please contact their Client Services Department at 1-888-841-6699.
If you have general questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
May 30, 2025 - Annual Provider Satisfaction Survey
In an effort to continue providing quality service to you, the physicians and staff serving our members, we are conducting a provider satisfaction survey through Press Ganey. Your feedback is important to understand how we impact your practice on a daily basis.
Provider offices were selected at random to complete this important survey. If your office receives a survey, we encourage you to take a few moments to complete and return it to Press Ganey. The feedback will help us provide better services to practices like yours.
Thank you in advance for your time and participation. If you have any questions regarding the survey, please do not hesitate to call Press Ganey at 1-800-558-1659.
May 27, 2025 - Closure of Rite Aid Pharmacies
We have learned that some Rite Aid Pharmacy locations across Pennsylvania could close their doors, which will affect prescriptions filled at these pharmacies by our Health Partners Plans/Jefferson Health Plans members.
Finding an Alternative Pharmacy
You or your patient can easily locate another local pharmacy using our online provider directory. To access the directory and find a complete list of participating pharmacies by ZIP code, please visit our Provider Directory page.
- Select the appropriate Plan Name, enter the ZIP Code, select “Pharmacy,” and click “Search Providers.”

Keep these points in mind when transferring prescriptions:
- Remaining refills. If there are refills left on the current prescription, patients may request a transfer from their Rite Aid pharmacy to another participating pharmacy.
- New prescriptions. When writing a new prescription, make sure it is submitted directly to the patient's new pharmacy.
- Closed before transfer. If the patient's Rite Aid pharmacy location closes before their prescription is transferred, a new prescription must be written.
We have also notified our impacted members of the potential Rite Aid closures. Our members may contact us for assistance finding a new in-network pharmacy by calling the number on the back of their Health Partners Plans/Jefferson Health Plans ID card.
If you have any questions, please call our Provider Services Helpline at 1-888-991-9023 (Monday – Friday, 9 a.m. – 5:30 p.m.).
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
May 22, 2025 - Key Pediatric Updates and Reminders for Well-Visits
We would like to inform you of several important updates and clarifications regarding well-visits and related services.
Key Updates and Reminders
- No Telehealth for Well-Visits:
- Effective January 1, 2025, telehealth services are no longer allowed for well-visits. All well-visits must be conducted in-person to ensure comprehensive care and adherence to clinical guidelines.
- Clarification on Timing Requirements for W15 and W30 Visit Reimbursement:
- Under 24 Months: There are no time restrictions for billing and reimbursement of well-visits for children under 24 months.
- 1-Year Well-Visit: The 1-year well-visit should be scheduled on or after the child’s first birthday to align with the vaccine schedule and clinical best practices.
- Sports Physicals vs. Well-Child Visits:
- Sports physicals are distinct from well-child visits. While both are important, they serve different purposes and should be billed accordingly.
- Sick Visits and Well-Child Visits on the Same Date:
- Sick visits and well-child visits can be conducted on the same date of service. This allows for efficient use of time and resources while ensuring comprehensive care.
- Annual Child and Adolescent Well-Visits:
- Well-visits can be conducted once per calendar year, even if 365 days have not yet passed. This annual visit is crucial for monitoring the child’s growth, development, and overall health. Providers will be reimbursed as long as it is a new calendar year.
Best Practices
The following tips and strategies can help your practice ensure members are seen for necessary well-visits and closing gaps in care:
- Combining Visits: If a patient comes in for a sick visit or sports physical and is due for a well-care visit, try to complete all services of a well-care visit during that time.
- Outreach Efforts: Prioritize outreach by targeting patients within the same household to achieve a greater impact.
- Comprehensive Care Gap Closure: Review all open care gaps for the patient and attempt to close them during the visit. Care gaps can be found on our provider portal.
Please note that these are recommendations only. For further guidance, kindly consult with your billing and compliance departments.
For more information on well-visits, vaccines, and improving performance, please visit our Pediatric Care Information page. The page has tip sheets, resource guides, policies, news updates, and more for our provider partners.
We appreciate your cooperation and commitment to providing high-quality care to our members. If you have any questions or need further assistance, please do not hesitate to contact us.
May 20, 2025 - Notification Regarding Memorial Day Holiday Hours
In observance of the Memorial Day on Monday, May 26, 2025, we will be closed.
Claim Payment Cycle – Business as usual for claim payment cycle.
Provider Helpline - Member eligibility/benefits as well as claim status inquiries can be accessed using the HealthTrio provider portal at hpplans.com/providers/provider-portals.
Pharmacy Call Center - All pharmacy calls will be forwarded to an outside service center with 24-hour access to an on-call pharmacist by contacting 1-866-841-7659.
Claims Reconsideration Call Center - Claims reconsideration requests can be submitted through the HealthTrio provider portal at hpplans.com/providers/provider-portals.
Utilization Management Call Center – closed with on-call services available by calling 1-866-500-4571. Authorization requests can be submitted through the HealthTrio provider portal hpplans.com/providers/provider-portals.
Enhanced Member Supports Unit Hotline – If members call in to the Enhanced Member Supports Unit, they will be prompted to leave a voicemail and they will receive a return call on the next business day. The Enhanced Member Supports Unit can be reached at 1-866-500-4571 (prompt 2, then prompt 7).
As always, we thank you for your continuing efforts to improve the health outcomes of our members.
May 13, 2025 - Annual D-SNP Model of Care Training - Required
Providers who have at least one Jefferson Health Plans Medicare Advantage Special (D-SNP) member assigned to their practice must have at least one person on their staff who is involved in the care of our dual-eligible special needs plan (D-SNP) members complete our annual D-SNP model of care training module. This training is required by the Centers for Medicare & Medicaid Services (CMS).
COLLABORATIVE CARE TEAM
As a vital member of our D-SNP care team, you help address the unique challenges of our members through a collaborative approach. To support this, all team members must complete a brief training on our D-SNP model of care to understand the program and their role within it.
COMPLETING THE ANNUAL D-SNP MODEL OF CARE TRAINING
To maintain compliance with CMS requirements, complete the course at hpplans.com/provider-online-courses within 30 days or join a 30-minute live webinar. The online course takes about 15 minutes. Register for the webinar at healthpartnersplans.com/webinars.
When you enter your tax ID in the attestation at the end of the online training, a drop-down will display all associated sites. Be sure to check off each site that you are attesting for before submitting your training attestation.
If you have questions, please contact ProviderEducation@jeffersonhealthplans.com or call the Provider Services Helpline at 1-888-991-9023 (M-F, 9 a.m. – 5:30 p.m.).
Thank you for your support in providing the highest quality of care for our members.
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
May 12, 2025 - 2025 Provider Manual
Our Provider manual has been updated for 2025 and is now available on our website at https://hpplans.com/providermanual.
As a reminder, the Provider Manual provides in-depth plan/product information on topics such as:
- Product/Benefit details for each Jefferson Health Plans’ product (Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, Jefferson Health Plans Individual and Family)
- Utilization, Quality Management and Clinical Programs
- Billing and Reimbursement regulations
- Guidelines for complaints, grievances and appeals
- Compliance requirements
- Much more!
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
May 12, 2025 - 2025 Access and Availability Survey
Each year, we survey our network to determine if our providers are meeting the access, appointment, and telephone availability standards, as set by the Department of Human Services (DHS) for Health Partners Plans Medicaid and Health Partners Plans CHIP members, and by the Centers for Medicare & Medicaid Services (CMS) for Jefferson Health Plans Medicare Advantage and Jefferson Health Plans Individual and Family Plans members.
The 2025 Provider Access, Appointment and Telephone Availability Standards Survey is now available. We ask that you complete this brief survey by Friday, June 13, 2025.
Please reference the letter faxed to your office on May 13, 2025 for your “Survey ID” number.
If you have any questions or are unsure of your Survey ID number, please send an email to AASurvey@jeffersonhealthplans.com.
April 23, 2025 - Medicare Member Wellness Rewards
We are continuing to offer Wellness Rewards, our rewards program, to all Jefferson Health Plans’ Medicare Advantage members in 2025. Wellness Rewards incentivize our members to complete specific health-related activities to earn rewards dollars on a reloadable flexible spending card. Please note that only Jefferson Health Plans’ Medicare members are eligible for the Medicare Wellness Rewards program.
Please refer to our website for a full listing of eligible health activities: www.HPPlans.com/rewards. Some health activities, such as medication adherence activities and preventive health screenings, are tied to current Quality Care Plus (QCP) measures. Jefferson Health Plans has found that encouraging patients to complete these activities may help improve performance on these QCP measures.
Overview of the Jefferson Health Plans’ Medicare Wellness Rewards Program:
- All eligible activities must be completed in 2025, and rewards must be redeemed in 2025.
- Members will receive a personalized letter in the mail listing all their 2025 eligible activities. Members will only be rewarded once for each eligible activity completed.
- If your patients have questions about Wellness Rewards, they should call Member Relations at 1-866-901-8000 (TTY 1-877-454-8477).
- To ensure that your patients are rewarded for their completed activities, please submit claims timely and correctly.
This is a sample image of the new Jefferson Health Plans Flex Card. This card will be loaded with Wellness Rewards, OTC allowances, and Flex benefit dollars for applicable members.
If you have any questions about the Wellness Rewards Program, please visit www.HPPlans.com/rewards.

Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
April 17, 2025 - Important Notice: Prior Authorization Platform Transition
We are currently in the process of transitioning to a new platform to better serve you. During this period, you may notice delays or temporary changes in how authorization requests are processed.
Please do not submit duplicate authorizations during this time as this may cause further delays. Our team is actively monitoring submissions and working diligently to ensure all requests are addressed promptly.
There will be downtime from Friday, April 18th at noon until Tuesday, April 22nd. During this time, we kindly request that urgent drug prior authorization be sent via fax to 866-240-3712.
We appreciate your patience and understanding as we work to improve our systems. If you have any urgent concerns, please contact the Provider Services Helpline. Thank you for your continued partnership.
March 27, 2025 - Continued Stay Request Form for Inpatient Acute Rehabilitation and Skilled Nursing Facilities (SNF)
Effective May 1, 2025, providers will be required to complete a Concurrent Review Request Form when requesting a continued stay at an inpatient acute rehabilitation or SNF. The form contains all required information to complete a medical necessity review.
The form can be downloaded from our website at www.healthpartnersplans.com/forms. Once completed, you must fax it to our UM Department at 215-991-4125.
This change applies to all lines of business – Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and Jefferson Health Plans Individual and Family Plans.
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
March 17, 2025 - MHK Prior Authorization Portal Training
As previously communicated, we are transitioning to the new MHK platform for prior authorization submissions, with the go-live date set for April 22, 2025.
We are hosting a series of live webinar trainings on Thursday, March 27, 2025, at 12:00p.m., Tuesday, April 1, 2025, at 12:00 p.m., and Wednesday, April 9, 2025, at 3:00 p.m.
Submission of authorization requests is a core function of MHK and can be used to submit inpatient admission, outpatient services (including DME), transportation, and home care requests. You will have direct access to view all your authorizations to check on the decision of those requests.
Effective April 22, 2025, fax submissions will no longer be accepted. All authorizations must be submitted through the portal.
As a reminder, the MHK platform will be accessible through the HealthTrio portal. There will be no change to the process for submitting requests through the EviCore portal.
To register for one of the upcoming webinars, visit HealthPartnersPlans.com/webinars and click “Registration.” You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
If you have any questions about this transition, please contact the Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. – 5:30 p.m.).
We hope that you will join us in our excitement about this upcoming change.
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
February 28, 2025 - Spring 2025 Provider Check Up Newsletter is Now Available!
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
The Spring edition of the Jefferson Health Plan’s provider newsletter, Provider Check Up, is now available on our website at https://hpplans.com/providernewsletter.
In this issue, we provide information on the following topics:
- 2025 Product ID cards
- Helping Patients Access Blood Pressure Cuffs
- CAHPS Season
- Preparing for New Medicare Measures
- And much more!
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
February 27, 2025 - Annual Training for Network Providers
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
We are hosting our first Annual Training Webinar of the year for network providers on Wednesday, March 12, 2025 at 12:30 p.m. All participating providers are required to demonstrate that they are knowledgeable and trained on important topics and participate in at least one webinar each year, offered on a quarterly basis. Participation in this webinar satisfies this annual requirement.
If you are newly contracted with our plan and would like a more comprehensive orientation, please contact us at providereducation@jeffersonhealthplans.com.
Topics Include:
Register Today
To register for this and future webinars, visit HealthPartnersPlans.com/webinars, select the webinar you are interested in attending and click the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
Alternate Option
While participation in this live webinar will satisfy your annual training requirement, there will be an alternative method to complete the training via online learning coming soon. More information will follow once the courses are available.
D-SNP Model of Care Training
Successful completion of the D-SNP Model of Care training module is mandatory for providers serving Jefferson Health Plans Medicare-Dual Eligible Special Needs Plan (D-SNP) members. At least one member of a care team location is required to take the annual online training course and distribute the training material to all D-SNP care team members.
The online training is currently being updated for 2025, more information will be available in the near future.
February 26, 2025 - In-Home Screenings--Provider Referral Process
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
We continue to partner with our vendor Healthy Measures to provide in-home screenings for noncompliant members for the following HEDIS measures: HbA1c Control, Kidney Function Evaluation, Diabetes Eye Exam, Controlling Blood Pressure, Lead Screening, and Osteoporosis Screening.
As you know, these services are often critical in helping to improve our members’ health outcomes, which helps your office improve quality performance and potentially increases your Quality Care Plus (QCP) revenue.
Once your office has identified the patients that are due for one of the above screenings, our Quality Improvement and Performance outreach team will coordinate the in-home appointment with your patient, typically within 30 days from the referral. Our outreach team will also complete reminder calls the day before for all appointments.
After an in-home appointment has been completed, your office will receive the results of the visit via fax from Healthy Measures. Results are sent approximately 2-3 weeks after the appointment was completed.
If you would like to refer a member and they agree to the in-home screening, please send an email to QIPReferrals@jeffersonhealthplans.com or contact Valerie Van Buren (vmcevoy@jeffersonhealthplans.com). Please include the following information: patient name, member ID, phone number, and test(s)/screening(s) needed.
If you have any questions, please contact the Provider Services Helpline at 1-888-991-9023(Monday – Friday, 9 a.m. – 5:30 p.m.).
February 26, 2025 - Annual Training for Ancillary Providers
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
We are hosting our first Annual Training for Ancillary Providers in 2025! The live webinar will be held on Wednesday, March 26, 2025, 12:30 – 1:30 p.m., tailored to the services provided by the provider types below:
|
|
This webinar will provide a comprehensive review of our administrative services and processes.
Topics include:
- 2025 updates
- Overview of online tools
- Claim filing instructions and best practices
- Credentialing
- Prior authorizations and Evicore
- Cultural Competency
REGISTRATION DETAILS
The webinar will be held on March 26, 2025, from 12:30 – 1:30 p.m. and will include a Q&A session. Webinars are free, but registration is required. Register now by going to HealthPartnersPlans.com/webinars. Select the webinar you are interested in attending and click the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
If you have any questions, call the Provider Services Helpline at 1-888-991-9023 (Monday – Friday, 9:00 a.m. - 5:30 p.m.) or email ProviderEducation@jeffersonhealthplans.com.
February 24, 2025 - Sleep Study Requirements Update
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
On August 6, 2024, we notified our provider network of a change in prior authorization requirements for sleep studies rendered in a facility setting. Effective with dates of service on or after February 15, 2025, sleep studies rendered in a facility setting will no longer require a prior authorization. This change affects all lines of business (Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, Jefferson Health Plans Individual and Family Plans).
No changes have been made to outpatient sleep studies, and they will continue to not require prior authorization.
Non-participating providers may require authorization as a condition of payment based on the member’s individual coverage. For information on products/services that require authorization as a condition of payment for out of network services, please contact the Utilization Management/Prior Authorization line at 1-866-500-4571, then select prompts 2 and 4.
Please submit prior authorization requests through our provider portal.
If you have any questions, please call our Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
February 20, 2025 - Referrals for In-Home Chronic Wound Care
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Effective March 3rd, 2025, providers can now refer patients with chronic wound care issues who are enrolled in Health Partners Plans Medicaid and Jefferson Health Plans Medicare Advantage Plans to Esperta Health.
Who is Esperta Health?
Esperta Health is a specialty physician practice that has partnered with us to deliver a complete wound care program for your patients with chronic wounds in the comfort of their home. This program ensures your patients/our members receive expert care from wound-certified specialists who can treat, heal, and prevent their chronic wound from recurring.
Chronic Wounds Approved for Referral:
*At-Risk Wounds: Multiple or Significant Patient Co-morbidities, Recurrent Infections, Prior Amputation(s), History of Wound-Related Hospitalization, Poor Nutrition, Weakened Immune System including: Chronic Illness such as cancer, diabetes, COPD, Immunosuppressant medications, including steroids and biologics.
How to Refer Patients to Esperta Health
As always, use secure and HIPAA-compliant means to transmit patient information:
- Fax the patient referral form to 615-278-1860;
- Refer online by going to espertahealth.com/referral;
- Call Esperta Health at 833-377-3782; or
- Send a secure email to customerservice@espertahealth.com.
For more information about Esperta Health, please visit espertahealth.com or contact our Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9:00 a.m. – 5:30 p.m.).
Thank you for your continued care of our members.
February 13, 2025 - MHK Prior Authorization Training Postponement
We are writing to inform you that due to unforeseen circumstances, the upcoming MHK Prior Authorization Portal Training scheduled for the following dates, February 19th, 21st and 26th will be postponed. We are currently working to reschedule the training and will provide you with new dates and times as soon as possible.
We apologize for any inconvenience this may cause and appreciate your understanding.
Please update your calendar accordingly.
If you have any questions, please contact us at providercommunications@jeffersonhealthplans.com
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
February 7, 2025 - COPD Med Optimization
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death worldwide.1
According to the GOLD Guidelines, goals for treatment of stable COPD include:
- Reducing symptoms
- Reducing risk (for the most recent GOLD Guideline recommendations, see https://goldcopd.org/2025-gold-report/)
Management of COPD should be individualized and based on symptom severity, risk of exacerbations, side-effects, comorbidities, and cost. However, single inhaler therapy has been shown to improve adherence to treatment.
The GOLD Guidelines utilize the ABE assessment in the chart below to evaluate a patient’s COPD based on current symptoms, airflow limitation, and history of exacerbation.
Care Guidelines
| Exacerbation history (per year) | ABE Group Assignment | |
|---|---|---|
| 2 moderate exacerbation or > 1 exacerbation leading to hospitalization | Group E: LABA+LAMA Preferred Drug List for LABA + LAMA includes: ANORO ELLIPTA, BEVESPI AEROSPHERE, STIOLTO RESPIMAT *consider LABA+LAMA+ICS if blood eos >300 Preferred Drug List for LABA + LAMA + ICS: TRELEGY ELLIPTA |
|
| 0 or 1 moderate exacerbation (not leading to hospitalization) | Symptoms: mMRC 0-1 or CAT<10 |
Symptoms: mMRC>2 or CAT > 10 |
Group A: Inhaled Bronchodilator Preferred Drug List Options include: |
Group B: LABA+LAMA (see above for formulary LABA + LAMA) |
|
Combination SABA+SAMA therapy is shown to be more effective than either agent alone in improving FEV1 and symptoms
- On formulary combination SABA+SAMA
- COMBIVENT RESPIMAT 20-100 MCG/ACT
Additional Patient Counseling Notes:
February 7, 2025 - MHK Provider Portal for Prior Authorization Submissions Training
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
As previously communicated, we are moving to a new platform, MHK, for prior authorization submissions. Go-live is scheduled for March 4, 2025.
Submission of authorization requests is a core function of MHK and can be used to submit inpatient admission, outpatient services (including DME), transportation, and home care requests. You will have direct access to view all your authorizations to check on the decision of those requests. In addition, supporting documentation can be uploaded to each request.
As a reminder, the MHK platform will be accessible through the HealthTrio portal. There will be no change to the process for submitting requests through the EviCore portal.
To assist with this transition, we will be hosting demonstration webinars of our new MHK prior authorization submission process, beginning on February 19:
February 19 at 12:00 p.m. |
To register for one of the upcoming webinars, visit HealthPartnersPlans.com/webinars and click “Register.” You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
If you have any questions about this transition, please contact the Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. – 5:30 p.m.).
We hope that you will join us in our excitement about this upcoming change.
February 5, 2025 - 2025 QCP Manual
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Thank you for your continued participation in our Quality Care Plus (QCP) program. QCP is designed to recognize and reward your practice’s performance in delivering high-quality services throughout the year. Every year, we assess the program to ensure a positive impact on both our members and our provider network.
The 2025 QCP Manual is now available on Jefferson Health Plans’ provider portal and at HPPlans.com/QCP. Please note that the manual will not be mailed to your office.
In November 2024, we shared updates to the 2025 QCP program with our provider network. Details of those updates can be found in this manual.
Your Provider Relations Representative will work closely with you to answer any questions and ensure that your office understands all 2025 changes. Thank you for your support in providing the highest quality of care to our members.
January 28, 2025 - MHK Provider Portal for Prior Authorization Submissions
In August 2024, we shared that we will be moving to a new platform, MHK, for prior authorization submissions. The original target date of December 1st, 2024 had been delayed, with a new target go live in March 2025.
As a reminder, the MHK platform will be accessible through the HealthTrio provider portal via a single sign on. There will be no change to the process for submitting requests through the EviCore portal.
Training materials, including both live and self-led learning courses, will be available as we move closer to our go live date. Please continue to check our Webinars page for announcements on upcoming trainings. In general, training videos and other resources on how to request access and how to navigate the HealthTrio provider portal are available at our Provider Portal page.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
January 15, 2025 - Notification Regarding Martin Luther King Jr. Day Holiday Hours
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
In observance of the Martin Luther King Jr. Holiday on Monday, January 20, 2025, we will not have modified hours of operations.
- Claim Payment Cycle - Claim payment cycle will kick off its normal schedule.
- Provider Services Helpline – Normal business hours. Member eligibility/benefits as well as claim status inquiries can be accessed using the provider portal. They can be reached at 1-888-991-9023.
- Pharmacy Call Center – Normal business hours (8 a.m. – 6 p.m.). All calls received after hours will be forwarded to an outside service center with 24-hour access to an on-call pharmacist. They can be reached at 1-866-841-7659.
- Claims Reconsideration Call Center – Normal business hours. Claims reconsideration requests can be submitted through the provider portal. They can be reached at 1-888-991-9023.
- Utilization Management Call Center - Normal business hours with on-call coverage only (1-866-500-4571). Authorization requests can be submitted through the provider portal.
- Enhanced Member Support Unit (EMSU) (Adult, Pediatric and Baby Partners Care Coordination) – Normal business hours (M-F 8 a.m. - 4:30 p.m.). All calls received after hours will be sent to voicemail throughout the holiday weekend. Voicemail messages will be responded to the next business day. EMSU can be reached at 1-866-500-4571 (prompt 2, then prompt 3).
As always, we thank you for your continuing efforts to improve the health outcomes of our members.
January 8, 2025 - PCMH 10-Day Follow-Up
As a requirement of the DHS Patient-Centered Medical Home (PCMH) program, patients admitted with an ambulatory sensitive condition must be seen by the primary care PCMH provider or specialist provider within ten days of discharge from the hospital. If the follow-up appointment takes place with a specialist, the specialist provider must share the patient’s follow-up visit notes with the primary care PCMH provider to meet this requirement.
This proactive approach contributes to reduced readmission rates, enhanced patient satisfaction with the care team and optimized health outcomes.
What’s Next?
- Review the below list of ambulatory sensitive conditions for which a post-discharge follow-up visit is required.
- Encourage your staff to schedule patients as soon as possible for post-hospitalization care appointments.
- Collaborate whenever possible with the primary care PCMH provider to effectively manage the patient’s ongoing plan of care.
We appreciate your ongoing commitment to the care of your patients and our members. If you have any questions, please contact the Provider Services Helpline at 1-888-991-9023. We are available Monday through Friday from 9 AM to 4:30 PM.
DRG |
Condition |
0053 |
Seizure |
0054 |
Migraine & Other Headaches |
0113 |
Infections Of Upper Respiratory Tract |
0137 |
Major Respiratory Infections & Inflammations |
0139 |
Other Pneumonia |
0140 |
Chronic Obstructive Pulmonary Disease |
0141 |
Asthma |
0191 |
Cardiac Catheterization W Circ Disord Exc Ischemic Heart Disease |
0192 |
Cardiac Catheterization For Ischemic Heart Disease |
0194 |
Heart Failure |
0198 |
Angina Pectoris & Coronary Atherosclerosis |
0199 |
Hypertension |
0203 |
Chest Pain |
0245 |
Inflammatory Bowel Disease |
0249 |
Non-Bacterial Gastroenteritis, Nausea & Vomiting |
0251 |
Abdominal Pain |
0304 |
Dorsal & Lumbar Fusion Proc Except For Curvature of Back |
0310 |
Intervertebral Disc Excision & Decompression |
0383 |
Cellulitis & Other Bacterial Skin Infections |
0420 |
Diabetes |
0422 |
Hypovolemia & Related Electrolyte Disorders |
0463 |
Kidney & Urinary Tract Infections |
0465 |
Urinary Stones & Acquired Upper Urinary Tract Obstruction |
0662 |
Sickle Cell Anemia Crisis |
0722 |
Fever |
Dec. 20, 2024 - Notification Regarding Holiday Hours and Claim Payment Cycle Change
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
In observance of the holidays, we will have modified hours of operation during the Christmas and New Years weeks.
- Claim Payment Cycle - Claim payment cycle will kick off its normal schedule.
- Provider Helpline - Closed December 25, 2024, and January 1, 2025. Member eligibility/benefits as well as claim status inquiries can be accessed using the HealthTrio provider portal at hpplans.com/providers/provider-portals.
- Pharmacy Call Center - December 24th, 2024, and December 31st Pharmacy hotline will close at 1pm. Closed on December 25, 2024, and January 1, 2025. All pharmacy calls will be forwarded to an outside service center with 24-hour access to an on-call pharmacist by contacting 1-866-841-7659.
- Claims Reconsideration Call Center - Closed on December 25, 2024, and January 1, 2025. Claims reconsideration requests can be submitted through the HealthTrio provider portal at hpplans.com/providers/provider-portals.
- Utilization Management Call Center - Will be closed December 25, 2024, and January 1, 2025, with on-call coverage only (1-866-500-4571) Authorization requests can be submitted through the HealthTrio provider portal hpplans.com/providers/provider-portals.
- Special Needs Unit (Adult, Pediatric and Baby Partners Care Coordination) - Modified business hours on December 24, 2024, and December 31, 2024, from 8:00 am – 3:00pm. Closed on December 25, 2024, and January 1, 2025. Calls after hours will be directed to our voice mail and will be returned as soon as possible on the next business day.
As always, we thank you for your continuing efforts to improve the health outcomes of our members and wish you a happy holiday.
December 3, 2024 - Provider Annual Orientation and Training Webinar Announcement Reminder
Jefferson Health Plans is hosting our 4th quarter Provider Orientation and Training Webinar on Wednesday, December 11, 2024. Jefferson Health Plans requires all participating providers to demonstrate that they are knowledgeable and trained on important topics and participate in at least one of four quarterly webinars each year. Participation in this webinar will satisfy this annual requirement.
This webinar will provide current and newly credentialed providers with a comprehensive review of Jefferson Health Plans’ benefits, administrative services, and processes.
Topics include important information for 2024 on:
- Health Partners Plans Medicaid and CHIP, Jefferson Health Plans Medicare Advantage and Individual and Family Plans
- Lab and other benefit carriers
- Online tools (including provider portal website, etc.)
- Claim filing instructions and best practices
- Community HealthChoices program
- Maternity services
- Access and availability standards
- Pay-for-Performance and Quality Care Plus
- EPSDT standards
- Special HIV/AIDS services
- Member identification cards
REGISTER TODAY
To register, select the webinar in the email message that you are interested in attending and click the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
ALTERNATE OPTION
While participation in this live webinar will satisfy your annual Jefferson Health Plans’ training requirement, there is an alternative method to complete the training. Please visit our Provider Online Courses page to access the Provider Orientation and Training eLearning course. Simply review with your staff and submit the electronic attestation found at the end of the training.
D-SNP MODEL OF CARE TRAINING
Successful completion of the D-SNP Model of Care training module is mandatory for providers serving Jefferson Health Plans Medicare-Dual Eligible Special Needs Plan (D-SNP) members. At least one member of a care team location is required to take the annual online training course and distribute the training material to all D-SNP care team members.
November 25, 2024 - Maternity Care Program Updates for 2025
We have successfully completed another year of the Maternity Quality Care Plus (MQCP) and the Obstetrical Needs Assessment Form (ONAF) Reimbursement programs, which are designed to recognize and reward your practice’s performance throughout the year.
November 25, 2024 - Winter 2024 Provider Checkup Newsletter is Now Available
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans. The Winter edition of the provider newsletter, Provider Checkup, is now available on our Provider Newsletter page.
In this issue, we provide information on the following topics:
- Important reminders on product naming
- Information on upcoming webinars
- QCP High Performers
- HEDIS, ONAF and other Quality information
- Important Clinical updates
- 2024 Pharmacy updates
- Dental information
- Cultural and Linguistic Requirements and Services and other administrative information
And much more!
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
November 25, 2024 - Prior Auths Changes for Cardiac, Transthoracic, and Transesophageal Echocardiogram Services
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Effective January 1, 2025, prior authorization will no longer be required for cardiac magnetic resonance imaging for the quantification of segmental dysfunction, transthoracic (TTE) and transesophageal (TEE) echocardiogram services for participating providers.
Certain cardiac services, including cardiac implantables (pacemakers and defibrillators), cardiac catherizations, and nuclear stress tests, will still require prior authorization and should continue to be submitted via eviCore.
This change applies to all of our lines of business (Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and Jefferson Health Plans Individual and Family Plans).
Non-participating providers may require authorization as a condition of payment based on the member's individual coverage. For information on products/services that require authorization as a condition of payment for out of network services, please contact the Utilization Management/Prior Authorization line at 1-866-500-4571, prompts 2, 4.
For specific code-level details, or if you have any questions, please visit our Prior Authorizations page or contact our Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9:00 a.m. – 5:30 p.m.).
November 21, 2024 - NJ Medicare Advantage PPO Plans: NEW Electronic Payor ID/PO Box
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Please be advised of the addition of a payor ID for the electronic submission of New Jersey Medicare Advantage PPO claims, as well as the mailing address for paper claims submissions. This will only apply to Jefferson Health Plans New Jersey Medicare Advantage PPO products; claims submission instructions will remain the same for all other Health Partners Plans’ and Jefferson Health Plans’ products.
Please note, Jefferson Health Plans recommends electronic claims submissions.
WHAT IS CHANGING
- ELECTRONIC PAYOR ID for New Jersey Medicare Advantage PPO: NJ099
- PAPER CLAIMS MAILING ADDRESS for New Jersey Medicare Advantage PPO:
Jefferson Health Plans
PO Box 211290
Eagan, MN 55121
WHAT REMAINS UNCHANGED
- ELECTRONIC PAYOR ID for Pennsylvania Medicare Advantage PPO: RP099
- PAPER CLAIMS MAILING ADDRESS for Pennsylvania Medicare Advantage PPO:
Jefferson Health Plans
PO Box 21921
Eagan, MN 55121
- ELECTRONIC PAYOR ID for ALL other products (Medicaid, CHIP, Medicare HMO/DSNP, Individual and Family Plans): 80142
- PAPER CLAIMS MAILING ADDRESS for ALL other products (Medicaid, CHIP, Medicare HMO/DSNP, Individual and Family Plans):
Jefferson Health Plans
PO Box 211123
Eagan, MN 55121
November 20, 2024 - Notice of Changes to the 2025 Jefferson Health Plans Medicare Part D Formularies
To help maintain high quality care while reducing health care expenditures to a sustainable level, we are implementing changes to our Medicare Part D formularies for the 2025 benefit year.
November 19, 2024 - Closing Gaps in Medication Adherence - Webinar Announcement
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
We would like to invite you to the Closing Gaps in Medication Adherence webinar presented by Temple. This webinar will discuss best practices related to medication adherence, that may lead to enhanced patient outcomes, lowered healthcare costs, and strengthened patient engagement. Temple will also highlight the critical role of their Outreach Specialists as well as how to access and utilize reports in HealthTrio.
Who should attend?
- Family Practice Providers
- Internal Medicine Providers
- Specialist Providers
- Care Teams
- Outreach Staff or Population Health Team Members
Registration Details
This 30-minute webinar will be held on Tuesday, December 3, 2024, at 12 p.m. There will be time for Open Discussion and Q&A after the presentation. You can register by clicking the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
Thank you for being a Jefferson Health Plans participating provider and for your partnership in serving our members.
November 14, 2024 - Important Notice: Taxonomy Billing Policy Update
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
This letter serves to notify the provider network of an update to billing requirements with regards to provider taxonomy codes. Effective January 1, 2025, all rendering providers are required to submit the Medicare-approved taxonomy in field locator 81 for paper claims or field locator 24J (Loop: 2310B – Rendering Provider Name) on the electronically submitted CMS 1500 claim.
This requirement applies to all Health Partners Plans/Jefferson Health Plans lines of business (Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, Jefferson Health Plans Individual and Family Plans).
Claims not billed with the appropriate taxonomy codes will be rejected or denied or may also result in reduced reimbursement.
If you have any questions, please contact the Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. – 5:30 p.m.).
November 13, 2024 - Quality Care Plus (QCP) Program Updates for 2025
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
We have important information to share about our Quality Care Plus (QCP) program, including an overview of updates for the 2025 QCP program.
2025 QCP Program Updates
Our QCP program rewards your practice’s performance for delivering quality services to our members. Each year, we assess the program to ensure that it positively affects our members and providers. We typically add and remove measures, as well as adjust the benchmarks and payment amounts based on historical performance, network performance, NCQA benchmarks, and CMS Stars benchmarks.
The changes outlined below will impact the 2025 measurement year (January 1 through December 31, 2025) and payments beginning in May 2026 (unless otherwise noted). Further clarification about how membership is calculated will be included in the QCP Manual.
Overall Program Changes
- Eligibility Requirement: Effective for the 2025 measurement period, providers will now be required to see at least 30% of paneled Medicaid members during the 2025 measurement year to participate and earn any incentive dollars for Medicaid measures beginning with the May 2026 payment cycle. Only members enrolled for at least 10 months at the site during the measurement year and remaining enrolled as of December 31 of the measurement year will be included in the rate calculation. Telehealth visits are allowed and will count toward the visit rate. This requirement impacts the Medicaid line of business only and will not affect the CHIP, Medicare Advantage, or Individual and Family Plans lines of business. This is a 5% increase from the previous years’ eligibility requirement; however, providers were given advanced notice of this planned increase as outlined in the 2024 QCP Manual and communicated throughout the year.
- Payment Calculation at the TIN Level: Effective for the 2024 measurement period (payments beginning in May 2025), providers will be measured and paid at the overall Tax Identification Number (TIN) level rather than the individual supplier location level. Providers will no longer need to meet a supplier location minimum membership threshold of 50 members. Only the TIN minimum membership threshold of 100 members must be met to participate.
- PMPMs based on Monthly Membership: Effective for the 2025 measurement period, incentives will be paid using a per member per month (PMPM) calculation, which is based on the current paneled membership of the practice every month.
2025 Quality Measure Changes
- Annual Wellness Visit*: This new Medicare measure will look at the percentage of Medicare members who had their annual wellness visit (preventive visit covered by Medicare) completed during the measurement year. Since this is not a Stars measure, we created custom benchmarks for this measure based on historical network performance.
- Care of Older Adults: In 2024, we included Medication Review and Pain Assessment as separate, stand-alone measures. In 2025, Functional Status Assessment will replace Pain Assessment. Functional Status Assessment and Medication Review will continue to be measured separately as stand-alone measures for Medicare only. Official CMS cut points are not available since Functional Status Assessment is a returning measure to the Stars program. Benchmarks will be based on historical network performance.
- Kidney Health Evaluation for Patients with Diabetes*: This new Medicare measure will look at the percentage of members 18-85 years of age with diabetes (type 1 and type 2) who received a kidney health evaluation, defined by an estimated glomerular filtration rate (eGFR), and a urine albumin-creatinine ratio (uACR), during the measurement year. Please note that members must complete both tests to be considered compliant for this measure.
- Oral Evaluation, Dental Services: This Medicaid only measure will be removed from the QCP program effective measurement year 2025. Dental providers will continue to be incentivized via our Dental P4P Program.
*Provider resource guides for these measures can be found on the Quality and Population Health page of our website. Additional details will also be provided in the 2025 QCP Manual.
Please click here for the complete list of the Medicare, Medicaid, and CHIP measures included in the 2025 program.
For More Information
The updated 2025 QCP Manual is expected to be released at the end of the year and will include all appropriate information. The 2025 QCP manual will be available at our Quality and Population Health page.
November 6, 2024 - Promoting Behavioral Health in a Primary Care Setting Webinar
Our collaboration with Magellan Healthcare webinar for tools you can use to deliver integrated quality care and coordinate behavioral healthcare for patients in a primary care setting. Magellan manages the behavioral health benefits for CHIP and Medicare Advantage members. Magellan is a leader in integrated, quality behavioral healthcare rooted in over 50 years of experience.
The webinar will cover topics including:
- Behavioral health (BH) conditions and how to refer to a BH provider
- Self-assessments and screening tools to screen for behavioral health conditions
- BH Quality HEDIS measures, including, but not limited to:
- Antidepressant Medication Management
- Follow-Up Care for Children Prescribed Medication for Attention Deficit Hyperactivity Disorder
- Follow-Up After Hospitalization for Mental Illness
- Initiation and Engagement of Alcohol & Other Drug Dependence Treatment
- Other available Magellan resources
Who should attend?
- Family Medicine Providers
- Pediatrics Providers
Registration details
This webinar will be held on November 20, 2024, at 12p.m. and will include time for your questions. Webinars are no cost, but registration is required.
If you have questions, contact providercommunications@jeffersonhealthplans.com or call the Provider Services Helpline at 1-888-991-9023 (M-F, 9 a.m. – 5:30 p.m.).
Thank you for your support in providing care for our members.
October 30, 2024 - Postpartum Care in Collaboration with Latino Connection
We are excited to tell you about a collaborative initiative with Latino Connection to provide additional support and outreach to Health Partners Plans Medicaid’s mothers and families in the postpartum period. Latino Connection is a leader in outreach and education specifically targeted at reaching low-income, underserved communities by creating programming and providing education focused on reaching families.
What is the goal of the partnership?
To provide comprehensive outreach and support to ensure the well-being of Health Partners Plans Medicaid members during the critical postpartum period. The aim of this program is to support women and families as well as improve postpartum visit rates.
Who qualifies for this visit?
Members due for a postpartum visit between 7 and 84 days after delivery.
What resources are provided by Latino Connection?
Latino Connection will assign two or more bilingual Community Health Workers (CHWs) to conduct outreach and home visits to members. The CHWs will:
- assist members with appointment coordination
- explain and help members to access benefits
- connect members with community-based resources, if needed
As you know, these services are critical in helping improve our members’ health outcomes, which also helps your office improve quality performance and potentially increases your Quality Care Plus (QCP) revenue.
We strongly believe that this partnership will be effective in improving compliance with health services, improve health outcomes for members, and identify health-related social needs. With your support, we can identify members’ needs and work together to improve their health outcomes and close care gaps.
If you or a member of your care team has any questions, please contact the Provider Services Helpline at 1-888-991-9023 (Monday – Friday, 9 a.m. – 5:30 p.m.).
As always, we appreciate your support in our mission to improve the health outcomes of our members.
October 25, 2024 - Medication Management Support for Medicare Advantage Members
We are committed to helping our Medicare members manage chronic conditions through medication support and adherence activities.
We would like to remind you that we have several resources to assist both you as providers and your patients in managing their medications. We partnered with several vendors and pharmacies that can help support our provider partners with outreach and medication adherence efforts. Our members also have access to pharmacy benefits through their specific health plan.
The resource guide can be found on our Resources for Medication Management and Adherence page. Please use it as a reference for medication support services for your patients.
Please contact Provider Services Helpline at 1-888-991-9023, (Monday – Friday, 9 a.m. – 5:30 p.m.) if you have any additional questions.
Thank you for your support in providing the highest quality of care to our members.
October 15, 2024 - New Shift Care Authorization Requirements
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid and CHIP plans, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Effective December 1,2024, we will begin requiring all Shift Care requests for Home Health Aide level of care to be submitted with all required modifiers listed on the request (U7, SC, TT modifiers). If the modifier is not included in the prior authorization request a U7 modifier will be included by default; an updated request will be required to add any additional modifiers. If you need to add or remove a modifier, please make sure to indicate the effective date, the days, and the hours for each modifier.
As a reminder, the SC modifier (Legal Responsible Relative to Staff) must be indicated on the physician referral in order to be included in the request.
Shift Care requests should continue to be submitted via the HealthTrio provider portal or faxed to the Shift Care team at 267-515-6667. Thank you for your attention.
October 14, 2024 - Medicare Home Care Utilization Review Process
Below is an overview of CMS regulatory requirements as it relates to the Medicare home care utilization review process. Jefferson Health Plans is now enforcing these requirements for Medicare Advantage members; compliance is necessary to avoid disruptions to prior authorization determinations.
October 9, 2024 - Branding Update (October 2024)
As a reminder, in July of 2023 we launched Jefferson Health Plans as our official marketing name for certain Health Partners Plans, Inc. products. While the marketing name changed for certain products, others did not. Our product names that remained the same (Health Partners Plans remained for the Medicaid and CHIP lines of business, while other products were with the Jefferson Health Plans marketing name for Medicare Advantage and the ACA/Individual and Family Plans lines of business).
As we move into 2025, please take note of our product names and member ID cards. It is important to know the differences in the product names and applicable program (Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare, Jefferson Health Plans Individual and Family) when speaking to our members/your patients.
Please see this PDF to see examples of our 2025 member ID cards. Any future changes to the ID cards will be communicated separately.
October 7, 2024 - Innovative Communication Strategies to Close Care Gaps Webinar
Jefferson Health Plans and Jefferson Health would like to invite you to an upcoming webinar, Innovative Communication Strategies to Close Care Gaps. The webinar will be held on October 29, 2024, at 12:00 p.m. Our experts will share best practice strategies to close gaps in care and drive improvements in quality metrics.
This webinar will provide a comprehensive look at the following:
- Strategies for effective gap closure including:
- Electronic communication campaigns
- Targeted centralized outreach
- Guided practice-based outreach
- Convenient screening locations
- Practice/Provider workflow optimization
Who should attend?
- Primary Care Providers
- Care Team Members
- Population Health Teams/Outreach Teams
- Care Coordination Teams
Webinar Registration Details
This is a no cost 30-minute webinar, but registration is required. This the second webinar in the Provider Best Practice Sharing series; future webinar topics will be communicated. If you are interested in contributing to a future presentation, please call us.
If you have questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.) or email providercommunications@jeffersonhealthplans.com.
We look forward to your participation and your continued commitment to remain up to date on Jefferson Health Plans resources and programs.
October 3, 2024 - Respiratory Illness Information
Respiratory illness season has officially begun, which runs during the fall and winter seasons. It’s important that all your patients be protected against respiratory illness during this season. According to the Centers for Disease Control and Prevention (CDC), health care providers are the most trusted source of health information for their patients. Immunization against influenza (flu), COVID-19, and respiratory syncytial virus (RSV) remains the best way to safeguard against hospitalizations, long-term health impacts, and death.
October 3, 2024 - Baby Partners Resources
We have developed a resource that provides more details about our Baby Partners program. This flyer can be shared within your office to all clinicians who interact with pregnant and postpartum members.
Click here to download the flyer.
Visit our Baby Partners information page for additional details about the program.
October 2, 2024 - HEDIS 2025 (Measurement Year 2024)
HEDIS reporting season is here! We need your support in collecting information from our members’ medical records for the 2024 reporting year.
The focus of Healthcare Effectiveness Data and Information Set (HEDIS) is to measure the health plan’s performance rather than individual provider performance. Participation with the HEDIS Project may assist in identifying gaps in care that are closed. Established by the National Committee for Quality Assurance (NCQA), annual HEDIS reporting is required of all HealthChoices plans by the Pennsylvania Department of Human Services and is necessary to maintain our NCQA accreditation.
Our Quality Management department has extensive experience in chart review and quality measurement. Registered nurses from this department will rely on your cooperation to arrange for the collection of the requested medical records needed for HEDIS reporting.
- We will continue our process to ensure this is an easy and safe process for your office.
- The preferred method of medical record collection is read-only access to your site’s EMR system for our staff members.
- We will coordinate with your office to identify the medical records needed for review.
- Please contact Pearl Taylor, HEDIS Coordinator, at 215-991-4283 or ptaylor@jeffersonhealthplans.comto discuss chart collection options.
- We will coordinate with your office staff on how to get requested records to reduce traffic in your office. If needed, a fax number and address will be provided in the request letter containing the member information.
- If necessary, our staff will arrange to visit your office to scan documentation to a secure laptop to avoid copying and transporting records.
As a friendly reminder, cooperation with our quality assurance efforts is part of your provider contract.
We look forward to working with your office with the goal of limiting the effect on your daily operations. Patient consent is not required for our request of medical records, as we are the payor/insurer provide services to your patients/our members.
If you have any questions, contact Pearl Taylor, HEDIS Coordinator, at 215-991-4283 or our Provider Services Helpline at 1-888-991-9023 (Monday-Friday, 9:00 a.m. to 5:30 p.m.).
September 27, 2024 - Medicare Advantage 2025 Product Overview Webinar Announcement
We invite you to an overview of our 2025 Medicare Advantage plans. Our Product Leadership Team will provide a general overview of each Medicare Advantage product and coverage areas, along with important information on our available tools and resources.
Who should attend?
- Family Practice Providers
- Internal Medicine Providers
- Specialist Providers
- Medical Billing Leadership
Registration Details
This 30-minute webinar will be held on Wednesday, October 2, 2024, at 12 p.m. Register by clicking the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
September 27, 2024 - Jefferson Health Plans Individual and Family Plans Webinar Announcement
We invite you to learn more about our 2025 Jefferson Health Plans Individual and Family Plans on Wednesday, October 9, 2024. Our Marketplace leadership team will provide an overview of our new and existing plans, expanded portfolio, improved cost sharing benefits and comprehensive benefits for members enrolled in our plans.
Who should attend?
- Family Practice Providers
- Internal Medicine Providers
- Specialist Providers
- Medical Billing Leadership
REGISTRATION DETAILS
The webinar will be held on Wednesday, October 9, 2024 at 12 p.m. Register by clicking the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
September 25, 2024 - Access to Care Plans for Medicare Advantage DSNP Members
In an effort to share information more effectively, effective October 1, 2024, Jefferson Health Plans Medicare Advantage DSNP member care plans will be available via the HealthTrio provider portal.
To access the member’s individual care plan report, please log into the HealthTrio provider portal and select “Document Manager”. In the “name” field, enter ICP@providerTaxID@memberfirstname.
Example: Sample Hospital (TIN: 11-1111111) searching for a Care Plan for member Jane Doe. The user would enter ICP@111111111@Jane in the Name field:
Training videos and other resources on how to request access and how to navigate the HealthTrio provider portal are available on our Provider Portal page.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
September 17, 2024 - Synagis Prior Authorizations
Jefferson Health Plans will start the annual Synagis® Prior Authorization process on October 16, 2024, two weeks before the respiratory syncytial virus (RSV) season begins. Synagis® (palivizumab) is a monoclonal antibody indicated to prevent a severe lower respiratory tract disease caused by RSV in infants and children at high risk. The RSV season begins November 1, 2024, and runs through March 31, 2025.
September 16, 2024 - LetsGetChecked In-Home Kit Mailing
Jefferson Health Plans continues to partner with LetsGetChecked to mail FOBT and/or a combination A1c/kidney health evaluation kit to Medicare Advantage members who are non-compliant with their colorectal cancer screening and/or diabetes management test. We also continue to send A1c kits to our Medicaid members who have not completed their A1c tests.
Your patients may receive one of the following kits:
Line of Business |
Kit Type |
JHP Medicare Advantage |
FOBT Kit |
JHP Medicare Advantage |
A1c/ Kidney Health Combination Kit |
HPP Medicaid |
A1c |
As you know, these services are often critical in helping improve our members’ health outcomes, which also helps your office improve quality performance and potentially increases your Quality Care Plus (QCP) revenue.
If your office receives a call from a patient inquiring about completing an in-home kit from LetsGetChecked, please encourage them to complete the test and mail it back as soon as possible. The kits come fully equipped with directions on how the patient can correctly collect the sample to ensure a valid result.
After an in-home kit has been completed, LetsGetChecked will provide your office with the lab results via mail. LetsGetChecked will also send the results to your patients. If your patient has an abnormal result, LetsGetChecked will attempt to reach out to the patient via telephone to encourage them to schedule an appointment and discuss the results with you.
We strongly believe that this effort by LetsGetChecked will be effective in improving compliance with health services. With your support, we can identify members’ needs and work together to improve their health outcomes and close care gaps.
If you or a member of your care team would like a list of your patients who will receive one of the kits in the mail or have any other questions, please contact the Provider Services Helpline at 1-888-991-9023 (Monday – Friday, 9 a.m. – 5:30 p.m.). As always, we appreciate your support in our mission to improve the health outcomes of our members.
August 28, 2024 - 2024 Wellness Rewards Reminder
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Earlier this year, Jefferson Health Plans notified providers of the Medicare Wellness Rewards program for our Medicare members. This is a reminder that members must complete all eligible health activities and rewards must be redeemed by December 31, 2024. Please note that our Medicare rewards program is different from the Medicaid/CHIP rewards Program.
You may see an increase in appointment requests toward the end of the year from members wishing to complete their activities and redeem their rewards by December 31, 2024.
To ensure that your patients are rewarded for their completed activities, please submit all claims timely and correctly. Our team may call your office during the fourth quarter to validate completed screenings to reward our members more quickly.
Please refer to the attached list for all eligible health activities and additional details on the rewards program. This information is also on our website, at www.HPPlans.com/rewards.
For questions about the Wellness Rewards program, Medicare members can contact Member Relations at 1-866-901-8000 (TTY 1-877-454-8477).
If you have any questions, please visit www.HPPlans.com/rewards.
Thank you for your continuous support in our effort to improve the health outcomes of our members.
August 28, 2024 - Annual Orientation and Training Webinar Announcement
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
Jefferson Health Plans is hosting our 3rd quarter provider orientation and training webinar on Wednesday, September 18, 2024. Jefferson Health Plans requires all participating providers to demonstrate that they are knowledgeable and trained on important topics and participate in at least one of four quarterly webinars each year. Participation in this webinar will satisfy this annual requirement.
This webinar will provide current and newly credentialed providers with a comprehensive review of Jefferson Health Plans’ benefits, administrative services, and processes.
Topics include important information for 2024 on:
- Health Partners Plans Medicaid and CHIP, Jefferson Health Plans Medicare Advantage and Individual and Family Plans
- Lab and other benefit carriers
- Online tools (including provider portal website, etc.)
- Claim filing instructions and best practices
- Community HealthChoices program
- Maternity services
- Access and availability standards
- Pay-for-Performance and Quality Care Plus
- EPSDT standards
- Special HIV/AIDS services
- Member identification cards
REGISTER TODAY
To register, select the webinar you are interested in attending and click the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
ALTERNATE OPTION
While participation in this live webinar will satisfy your annual Jefferson Health Plans’ training requirement, there is an alternative method to complete the training. Please visit the Provider Online Courses page to access the Provider Orientation and Training eLearning course. Simply review with your staff and submit the electronic attestation found at the end of the training.
D-SNP MODEL OF CARE TRAINING
Successful completion of the D-SNP Model of Care training module is mandatory for providers serving Jefferson Health Plans Medicare-Dual Eligible Special Needs Plan (D-SNP) members. At least one member of a care team location is required to take the annual online training course and distribute the training material to all D-SNP care team members.
After taking the training, go to the Provider Education Attestation page and complete the attestation form.
ACCESS AND APPOINTMENT & AVAILABILITY STANDARDS
Timely access to quality health care is extremely important for our members. As you should be aware, it is a regulatory requirement that all Jefferson Health Plans participating providers must meet clearly defined access, appointment, and availability standards. These standards can be found in Chapter 11: Provider Practice Standards & Guidelines of the Jefferson Health Plans Provider Manual, available by going to the Provider Manual page.
Each year, Jefferson Health Plans surveys our providers to determine if they are meeting these standards. The mandatory survey launched on April 30th. If you haven’t already done so, please use the link or QR code to complete this survey to ensure you are meeting regulatory requirements.
https://healthpartnersplans.az1.qualtrics.com/jfe/form/SV_6KBk55KDjJMBI4S
August 22, 2024 - Fall 2024 Provider Checkup Newsletter is Now Available!
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans. The Fall edition of the Jefferson Health Plans provider newsletter, Provider Checkup, is now available on our website at our Provider Newsletter page.
In this issue, we provide information on the following topics:
- 2024 Webinar series information
- Access and Availability Survey reminders
- Information on Quality programs/initiatives
- Pharmacy Formulary Changes
- Dental Topics
- Policy Bulletin Updates
And much more!
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
August 21, 2024 - Introduction to MHK/Portal Mandate for Prior Authorization Requests
Thank you for being a valued provider for members in one or more of our health plans: Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, and/or Jefferson Health Plans Individual and Family Plans.
We wanted to share some exciting news! Jefferson Health Plans will be moving to a new platform, MHK, for prior authorization submissions with a target go live date of December 1, 2024. The MHK platform will be accessible through the HealthTrio provider portal through a single sign on. There will be no change to the process for submitting requests through the EviCore portal.
With the shift to the MHK platform, and in a continued effort to share information via sustainable means, effective February 1, 2025, providers will also be required to submit requests for prior authorizations electronically via MHK.
Additionally, looking ahead later into 2025, Jefferson Health Plans will be moving to the electronic distribution of the Inpatient Authorization Determination Logs. Hospitals will need to utilize the HealthTrio provider portal to retrieve these daily reports. We will provide additional information as our internal processes are finalized.
Training videos and other resources on how to request access and how to navigate the HealthTrio provider portal are available at the Provider Portal page.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
August 9, 2024 - You're Invited: HCV Treatment, Monitoring, and Adherence Webinar
Thank you for being a Jefferson Health Plans participating provider. We’d like to invite you to an upcoming webinar, Hepatitis C Virus (HCV) Treatment, Monitoring and Adherence. The webinar will be held on August 21 at 12:00 p.m.
The Centers for Disease Control and Prevention (CDC) now recommends universal Hepatitis C screening for all adults and pregnant women. Jefferson Health Plans has partnered with Gilead Sciences to present current guidelines for screening, treatment, monitoring, and adherence of HCV.
This webinar will cover the following topics:
- AASLD simplified treatment guidelines
- Minimal monitoring requirements
- Adherence and high rates of cure
- Treatment as prevention to eliminate HCV
- Discussion of best practices with time for Q&A
Webinar Registration Details
This free 60-minute webinar is August 21, from 12:00 p.m. to 1:00 p.m. All primary care providers are encouraged to attend.
If you have questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.) or email providercommunications@jeffersonhealthplans.com.
We look forward to your participation and your continued commitment to remain up to date on Jefferson Health Plans resources and programs.
August 9, 2024 - Health Partners Plans CHIP - Removal of Prior Authorization Requirements for PT/OT/ST
Thank you for being a valued participating provider. We are writing to inform you of an important update to the prior authorization requirements for our Health Partners Plans CHIP product.
Effective October 1, 2024, Health Partners Plans CHIP will no longer require prior authorization for Physical Therapy (PT), Occupational Therapy (OT) and Speech Therapy (ST) services for CHIP members when provided by a participating provider.
Prior authorization guidelines must be followed for PT, OT, ST services for all other products (Health Partners Plans Medicaid, Jefferson Health Plans Medicare Advantage and Individual and Family Plans), and for all non-participating providers.
If you have any questions, please visit the prior authorization page of our website at healthpartnersplans.com/providers/prior-authorization, or contact our Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9:00 a.m. – 5:30 p.m.).
August 8, 2024 - Duplicate Claims Payment
Jefferson Health Plans recently received an unusually high volume of claims through our clearinghouse, SDS. These claims were submitted to SDS through another trading partner and included a high volume of duplicate claims. Certain claims were inadvertently adjudicated to pay, resulting in duplicate payments being made to providers. As you know, our participating agreements and provider manual call for our recoupment of these incorrect payments.
We will begin retracting the duplicate payments beginning the week of August 12, 2024. We expect the full recovery effort to be completed by September 17. You will be able to see the impacted claims on your weekly remittance advice. Thank you for your kind attention to this matter.
August 7, 2024 - Update to Prior Authorization Requirements - Sleep Studies
In an effort to reduce the administrative burden around prior authorization requests, effective October 1, 2024, Jefferson Health Plans will no longer require prior authorization for Sleep Studies when rendered outside of a facility setting for all lines of business (Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, Jefferson Health Plans Individual and Family Plans).
Sleep studies rendered in the facility setting (POS 19, 22, 49) will still require a prior authorization. Effective with this above change, as of October 1, 2024, prior authorization requests for sleep studies will no longer be submitted to eviCore. Please submit all prior authorization requests to Jefferson Health Plans via the HealthTrio provider portal.
The link to access the HealthTrio portal, along with portal training resources can be found on our website at our Provider Portal page.
If you have any questions, please call our Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
July 12, 2024 - Department of Human Services Mobile Clinic Survey
Health Partners Plans and Jefferson Health Plans, on behalf of the Pennsylvania Department of Human Services (DHS), would like to announce the launch of a survey DHS is conducting to gather more information on Mobile Health Clinics.
If your organization operates a mobile clinic, please take 5 to 7 minutes to complete this survey. The results of this survey will help DHS describe the current breadth of mobile services provided across the state, identify interest in collaboration among mobile service providers to share best practices and identify unmet needs/resources, and identify opportunities to promote and support the mobile clinics, including opportunities for expansion of services.
For this survey, a mobile clinic is defined as a customized motor vehicle that travels to communities to provide health care, including medical, dental, behavioral health, and substance use services. They may be staffed by physicians, advance practice providers, dentists or dental hygienists, nurses, community health workers, and other health professionals.
Please use this link to complete the survey: https://sst.qualtrics.com/jfe/form/SV_3VmJrsKQ5HCiKNg. Please contact DHS directly with questions.
June 28, 2024 - Newborn Stay Authorization Policy Update
Jefferson Health Plans is revising our authorization policy for obstetrical delivery and NICU nursery care. In July 2021, Jefferson Health Plans implemented an authorization policy that allowed certain NICU and newborn AP-DRG codes to pay without requiring authorization. Effective September 1, 2024, we will be sunsetting this policy and will require all NICU and/or detained newborn admissions to require an authorization.
With the change to this policy, NICU admissions and/or detained newborn admissions (billed with any applicable revenue code(s)) will require an authorization for payment.
Prior authorization requests should be submitted via the HealthTrio provider portal. Please visit the Provider Portal page for access, training material and resources.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
June 25, 2024 - Complete Required Annual D-SNP Model of Care Training by July 25
Thank you for being a participating Jefferson Health Plans provider. If your practice has at least one Jefferson Health Plans Medicare Advantage Special (D-SNP) member assigned to your practice, at least one person on your staff who is involved in the care of our dual-eligible special needs plan (D-SNP) members must complete our annual D-SNP model of care training module. This training is required by the Centers for Medicare & Medicaid Services (CMS).
COLLABORATIVE CARE TEAM
You play a crucial role on the care team that serves our D-SNP members. Our collaborative care team approach helps you take on the unique and complex challenges presented by these members. All care team members must take this brief but effective training on our D-SNP model of care program. Our goal is to ensure that every care team member understands how the program works and their role.
COMPLETING THE ANNUAL D-SNP MODEL OF CARE TRAINING
To maintain compliance with CMS requirements, you can complete this course within 30 days of receiving your letter or attend the live webinar. Completing online should not take more than 15 minutes and via webinar 30 minutes.
When you enter your tax ID in the attestation at the end of the online training, a drop-down will display all associated sites. Be sure to check off each site that you are attesting for before submitting your training attestation.
If you have questions, please contact ProviderEducation@hpplans.com or call the Provider Services Helpline at 1-888-991-9023 (M-F, 9 a.m. – 5:30 p.m.).
Thank you for your support in providing the highest quality of care for our members.
June 21, 2024 - Quality Reports Calendar, KED, TRC, and Hypertension Best Practices Tip Sheets
Thank you for being a valued participating provider. Continuing with our commitment to ensure providers have the resources available to provide the highest quality of care to our members, the Quality Reports Calendar, Kidney Health Evaluation for Patients with Diabetes (KED), Transitions to Care (TRC), and Hypertension Clinical Best Practices tip sheets are now available on our website!
The Quality Reports Calendar is a yearly overview of the various quality reports, and the availability of those reports to providers as it relates to QCP, MQCP, STARs, HEDIS and other Quality initiatives. You can find a downloadable copy of the calendar on our Quality and Population Health page.
The KED and TRC tip sheets, while primarily focused on the Medicare population, contain valuable information that can apply to members across all of Jefferson Health Plans’ product lines.
The Hypertension clinical best practices tip sheet provides valuable information on the treatment of Hypertension, specifically within the African-American population.
These tip sheets, calendars and more can be found on the Quality and Population Health information page.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
June 12, 2024 - You're Invited: Improving Engagement Through Well Visit Events Webinar
Thank you for being a Jefferson Health Plans participating provider. We’d like to invite you to an upcoming webinar, Improving Engagement Through Well Visit Events, presented in partnership with CHOP. The webinar will be held on Tuesday, June 25 at 12:00 p.m.
Jefferson Health Plans has partnered with Steve Callum, MBA, LSSGB, PCMH CCE, Senior Manager Value-Based Care with the Children’s Hospital of Philadelphia (CHOP), to provide an overview of CHOP’s approach to improving pediatric well-child visits to close care gaps and improve the influence of health and development of their pediatric population through a series of fun and engaging events. There will be a brief presentation, with time allowed for provider questions:
- What is a Well Visit Event?
- Why does CHOP do this?
- How can you create your own?
Webinar Registration Details
The free 30-minute webinar will be held on Tuesday, June 25, from 12:00 p.m. to 12:30 p.m. All primary care providers are encouraged to attend. This is the first webinar in the Provider Best Practice Sharing series; future webinar topics will be communicated. If you are interested in contributing to a future presentation, please call us.
If you have questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.) or email providercommunications@jeffersonhealthplans.com.
We look forward to your participation and your continued commitment to remain up to date on Jefferson Health Plans resources and programs.
June 12, 2024 - Fluticasone HFA - Update to Preferred Drug List (PDL)
Thank you for your continuing efforts to improve the health outcomes of our members. On January 18, 2024, you were advised that GlaxoSmithKline (GSK) has discontinued manufacturing Flovent HFA and Diskus as of December 31, 2023, and were provided a list of preferred drug alternatives.
Effective April 29, 2024, Fluticasone Propionate HFA has been added to the Statewide PDL for Medicaid patients and is now included as a preferred alternative for children 7 years of age and younger without a prior authorization. **As of 6/19/2024, the Department of Human Services (DHS), has updated the age range for children 12 years of age and younger**.
As a reminder, below is a full list of the preferred drug list alternatives:
- Arnuity Ellipta
- Asmanex HFA
- Asmanex Twisthaler
- Budesonide 0.25 mg/2 ml, 0.5 mg/2 ml
- Pulmicort Respule
- Pulmicort Flexhaler
- Qvar Redihaler
- Arnuity Ellipta
- Fluticasone HFA
For the most up-to-date information regarding Jefferson Health Plans’ formularies, please visit our Formularies page. For more information, call our Pharmacy department at 215-991-4300 or our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.).
Thank you for your cooperation in improving the quality of care you deliver to your patients and our members.
June 11, 2024 - Provider Annual Orientation and Training Webinar Announcement for 2024
Thank you for being a valued participating provider. Jefferson Health Plans is hosting our Quarter 2 provider orientation and training webinar on June 19, 2024. Jefferson Health Plans requires all participating providers to demonstrate that they are knowledgeable and trained on important topics and participate in at least one of four quarterly webinars each year. Participation in this webinar will satisfy this annual requirement.
This webinar will provide current and newly credentialed providers with a comprehensive review of Jefferson Health Plans’ benefits, administrative services, and processes.
Topics include important information for 2024 on:
- Health Partners (Medicaid), KidzPartners (CHIP),Jefferson Health Plans Medicare Advantage and Individual and Family plans
- Lab and other benefit carriers
- Online tools (including provider portal website, etc.)
- Claim filing instructions and best practices
- Community HealthChoices program
- Maternity services
- Access and availability standards
- Pay-for-Performance and Quality Care Plus
- EPSDT standards
- Special HIV/AIDS services
- Member identification cards
REGISTER TODAY
To register, select the webinar you are interested in attending and click the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
ALTERNATE OPTION
While participation in this live webinar will satisfy your annual Jefferson Health Plans’ training requirement, there is an alternative method to complete the training. Visit the Provider Online Courses page to access the Orientation and Training eLearning course. Simply review with your staff and submit the electronic attestation found at the end of the training.
D-SNP MODEL OF CARE TRAINING
Successful completion of the D-SNP Model of Care training module is mandatory for providers serving Jefferson Health Plans Medicare-Dual Eligible Special Needs Plan (D-SNP) members. At least one member of a care team location is required to take the annual online training course and distribute the training material to all D-SNP care team members.
To take the training, go to the Provider Online Courses page. When training is complete, go to the Provider Education Attestation page to confirm your participation.
ACCESS AND APPOINTMENT & AVAILABILITY STANDARDS
Timely access to quality health care is extremely important for our members. As you should be aware, it is a regulatory requirement that all Jefferson Health Plans participating providers must meet clearly defined access, appointment, and availability standards. These standards can be found in Chapter 11: Provider Practice Standards & Guidelines of the Jefferson Health Plans Provider Manual.
To help ensure that your site is adhering to appropriate timeframes for scheduling and availability, we have enclosed copies of these standards for PCPs, Specialists and OB/GYNs. These documents include:
- Provider Access and Appointment Standards
- Telephone Availability Standards
JEFFERSON HEALTH PLANS ACCESS AND AVAILABILITY SURVEYS
Each year, Jefferson Health Plans surveys our providers to determine if they are meeting these standards. The mandatory survey launched on April 30. We look forward to your participation.
Thank you for your support in providing the highest quality of care for our members.
June 11, 2024 - Provider Manual 2024 Update
Thank you for being a valued participating provider. The Jefferson Health Plans’ Provider Manual, updated for 2024, has been finalized and is now available on our website.
As a reminder, the Provider Manual provides in-depth plan/product information on topics such as:
- Product/Benefit details for each Jefferson Health Plans’ product (Health Partners Plans Medicaid, Health Partners Plans CHIP, Jefferson Health Plans Medicare Advantage, Jefferson Health Plans Individual and Family)
- Utilization, Quality Management and Clinical Programs
- Billing and Reimbursement regulations
- Guidelines for complaints, grievances and appeals
- Compliance requirements
- Much more!
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
May 29, 2024 - Prior Authorization Update - CHIP
Thank you for being a valued Jefferson Health Plans provider. We are writing to inform you of an important update to the prior authorization requirements for our Health Partners Plans CHIP (KidzPartners) product.
Effective June 1, 2024, Jefferson Health Plans will no longer require prior authorization requirements for Ambulatory Surgical (ASC), Short Procedure Unit (SPU), and Outpatient Surgical services for our CHIP members. This applies to all services billed in POS 22 and 24 and/or Revenue code 360 and 361, for dates of service beginning on/after June 1, 2024.
If you have any questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9:00 a.m. – 5:30 p.m.).
May 21, 2024 - You're Invited: Care Coordination Support for You and Your Patients Webinar
We’d like to invite you to an upcoming webinar, Care Coordination Support for You and Your Patients. The webinar will be held on June 5 at 12:30 p.m.
Our clinical programs can support your practice and your Health Partners Plans (Medicaid) and Health Partners Plans KidzPartners (CHIP) patients. These programs help drive Healthcare Effectiveness Data and Information Sets (HEDIS) in a positive direction, which ties to your Quality Care Plus (QCP) reimbursement and overall quality of care you provide.
This webinar will provide a comprehensive look at our clinical programs and resources, including:
- Clinical Connections, which conducts appropriate patient follow-up following a health risk assessment and after a hospital discharge to ensure a patient’s safe transition to their home.
- Baby Partners, which offers coordination of care for pregnant members throughout pregnancy and 84 days after delivery.
- Pediatric Care Coordination for children up to age 21, which provides reminders for parents and guardians to ensure patients receive appropriate screenings with guidance from the EPSDT/Bright Future requirements, including help for children with high lead levels, high risk asthma, developmental delays, NICU graduates and children with complex needs.
- Adult Care Coordination for patients (age 21 and older) with a disability or chronic condition.
Webinar Registration Details
The free 30-minute webinar is June 5, from 12:30 p.m. to 1:00 p.m.
If you have questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.) or email providercommunications@jeffersonhealthplans.com.
We look forward to your participation and your continued commitment to remain up to date on Jefferson Health Plans resources and programs.
May 21, 2024 - CAHPS and HOS Guidebook Updates
Jefferson Health Plans is focusing on improving patient satisfaction scores and elevating patients’ experience with their health plan and their providers.
Jefferson Health Plans is committed to partnering with our network providers to elevate patient satisfaction and improve the in-office experience. This guidebook will cover multiple facets of patient experience, including:
- Consumer Assessment of Healthcare Providers and Systems (CAHPS)
- Health Outcomes Survey (HOS)
- Best practices and tips to optimize the patient experience
The resource guide can be found here on our website. If you have any questions about this resource and its contents, please contact our Provider Services Helpline at 1-888-991-9023, (Monday – Friday, 9 a.m. – 5:30 p.m.).
May 17, 2024 - Summer 2024 Provider Check-Up Newsletter is Now Available
The Summer edition of the Jefferson Health Plans’ provider newsletter, Provider Check Up, is now available on our Provider Newsletters page.
In this issue, we provide information on the following topics:
- Change HealthCare Cyber Security Incident updates
- Information on upcoming webinars
- HEDIS, ONAF and other Quality information
- Important Clinical updates
- 2024 Pharmacy updates
- Dental information
- Cultural and Linguistic Requirements and Services and other administrative information
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
April 29, 2024 - 2024 Provider Access, Appointment and Telephone Availability Standards Survey is Now Available
Each year, Jefferson Health Plans surveys our network to determine if providers are meeting the Access and Appointment Standards and Telephone Availability Standards as set by the Department of Human Services (DHS) for Health Partners (Medicaid) and KidzPartners (CHIP) members, and by the Centers for Medicare & Medicaid Services (CMS) for Health Partners Medicare members.
The 2024 Provider Access, Appointment and Telephone Availability Standards Survey is now available. We ask that you complete this brief survey by May 13, 2024.
Please reference the letter that was faxed to your office on April 29, 2024 for your “Survey ID” number.
If you have any questions or are unsure of your Survey ID number, please send an email to AASurvey@jeffersonhealthplans.com.
April 26, 2024 - Bariatric Policy Change
Elective Laparoscopic Sleeve Gastrectomy – Updates to Authorization Guidelines
Thank you for being a valued participating provider. This letter is to inform you of an important change related to Elective Laparoscopic Sleeve Gastrectomy procedures for our Health Partners (Medicaid) and KidzPartners (CHIP) members.
Effective 7/1/2024, Elective Laparoscopic Sleeve Gastrectomy (CPT 43775), will no longer be automatically approved in an inpatient setting. We will follow the current InterQual guidelines regarding prior authorization inclusion criteria which are aligned with recommendations from the American Society of Metabolic and Bariatric Surgery.
InterQual criteria recognizes that many of these cases can be managed in the outpatient setting and has become the standard of care. If an Inpatient stay is requested at the time of preauthorization, the case will be reviewed by a Medical Director. If an outpatient setting is requested, the case will only be reviewed against the current InterQual criteria. Cases that are preauthorized and approved as an outpatient procedure that subsequently develop post-operative complications and require a prolonged stay will require additional clinical information. An inpatient stay can be requested by the provider at that time.
This change affects the Health Partners (Medicaid) and KidzPartners (CHIP) plans. The Jefferson Health Plans Medicare line of business will not be affected, and this continues to be a non-covered service for the Individual and Family Plans.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
April 5, 2024 - Updates to APR DRG Version
Thank you for being a participating provider with Jefferson Health Plans. This letter contains important information about the update to the current version of APR-DRG.
In accordance with the Pennsylvania Department of Human Services (DHS) and per Jefferson Health Plans’ policy RB.028.A, Jefferson Health Plans moved from APR-DRG version 39 to APR-DRG version 41, effective February 16, 2024. The policy can be found at our Policy Bulletin Library page.
Claims received as of April 4, 2024, with service dates on or after February 16, 2024 will be processed on APR-DRG version 41.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
April 4, 2024 - Self-Monitoring Blood Pressure Cuffs for Pregnant Members
According to the Center for Disease Control and Prevention (CDC), 1 in every 12 to 17 pregnancies among women ages 20 to 44 in the U.S. experience high blood pressure. In addition, CDC data shows that black women are two to three times more likely to die from pregnancy-related complications than white women. High blood pressure can cause problems throughout the pregnancy, during delivery and postpartum. However, high blood pressure can be preventable and treatable.
How to order free blood pressure cuffs for pregnant Health Partners members
All Health Partners (Medicaid) pregnant members, regardless of age, are eligible for a blood pressure cuff with a provider script once per calendar year. We encourage providers to write scripts for their patients’ blood pressure cuff equipment and have them bring the equipment into the office to ensure proper use throughout their pregnancy and 1-year post-partum period. Use the blood pressure monitor referral form at our Form and Supply Requests page.
Based on the American College of Obstetricians and Gynecologists guidelines, blood pressure standards are as follows.
- Normal: Less than 120/80 mm Hg
- Elevated: Systolic between 120-and 129-mm Hg and diastolic less than 80-mm Hg
- Stage 1 hypertension: Systolic between 130-and 139-mm Hg or diastolic between 80-and 89-mm Hg
- Stage 2 hypertension: Systolic at least 140-mm Hg or diastolic at least 90-mm Hg
Maternity providers play an important role in educating their patients to achieve optimal health through health education and self-management tools. Health Partners (Medicaid) has developed a blood pressure initiative that is aimed to assist maternity providers with educating their pregnant patients on the importance of self-monitoring blood pressure, how to use blood pressure equipment, sharing results with their clinicians, and increasing their knowledge about possible complications of hypertension.
For billing, use code 99473: Self-measured blood pressure using a device validated for clinical accuracy; patient education/training and device calibration.
This link to an infographic on how to take their blood pressure can be shared with your patients:
Thank you for being a participating provider.
March 29, 2024 - Jefferson Health Plans and You: Enhancing Patient Experience Webinar
Jefferson Health Plans is hosting a webinar in collaboration with ProspHire, a healthcare focused management consulting firm, that will focus on the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Survey and best practices recommendations from across the industry. We invite you and your team to participate in the webinar on Wednesday, April 17, 2024.
Our goal is supporting practices like yours in optimizing the patient experience. Member satisfaction is a leading indicator in measuring overall quality of care and patient engagement. This webinar is ideal for anyone involved in patient care and experience. Whether you are looking to understand more about CAHPS or seeking ways to improve, this session will provide valuable insights and practical strategies for your office to implement.
The upcoming webinar will cover the following topics:
- Understanding CAHPS and its importance to Health plan quality.
- Best practices and industry insights.
- Jefferson Health Plans’ resources for member satisfaction and customer service.
- Q&A and sharing ideas and best practices from a provider perspective.
We encourage the following roles within your organization to participate in the webinar:
- Clinical and non-clinical leadership team
- Clinical and non-clinical staff involved in quality improvement projects
- Clinical and non-clinical staff involved in member satisfaction initiatives
REGISTER NOW
This webinar will be held on April 17 at 12:00 p.m. Webinars are free, but registration is required.
If you have questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday – Friday, 9:00 a.m. – 5:30 p.m.) or email ProviderCommunications@jeffersonhealthplans.com.
Thank you for being a Jefferson Health Plans participating provider and for your anticipated partnership in providing great service to our members.
March 22, 2024 - Quality Initiatives, Opportunities and Resources Webinar
Thank you for being a participating Jefferson Health Plans provider. You’re invited to participate in an upcoming webinar on Quality Initiatives, Opportunities and Resources on April 10, 2024.
This webinar will offer insight from Jefferson Health Plans subject matter experts on all things quality; from tips to help improve members’ medication adherence, updates on Jefferson Health Plans’ planned quality initiatives in 2024 and recommendations for reporting and resources providers should be utilizing.
Valerie Van Buren, Director of Quality Improvement and Performance, and Terry McKeever, Director of Quality Management, will be the lead presenters. The webinar will cover topics including:
- Quality “hot topics”
- Medication adherence
- Jefferson Health Plans’ vendor and community partnerships
- Provider Incentive Program: QCP 2024 program updates
- HEDIS measures, reporting and available resources
Who should attend?
- Clinical and non-clinical leadership team
- Clinical and non-clinical staff involved in quality improvement projects
- Staff managing the P4P revenue cycle opportunities from your MCO partners
- Staff reviewing and utilizing the Jefferson Health Plans reports on Health Trio
Registration Details
This webinar will be held on April 10, 2024, from 12-1 p.m. and will include a Q&A session. Webinars are free, but registration is required.
If you have any questions, call the Provider Services Helpline at 1-888-991-9023 (Monday–Friday, 9 a.m. to 5:30 p.m.) or email ProviderCommunications@jeffersonhealthplans.com.
March 15, 2024 - Smart Data Solutions Clearinghouse
Jefferson Health Plans has entered a partnership with Smart Data Solutions (SDS) Clearinghouse to accommodate Electronic Data Interchange (EDI) claim submissions for our two Payor IDs:
- Health Partners (Medicaid)/KidzPartners(CHIP)/Jefferson Health Plans Medicare HMO/Jefferson Health Plans Individuals and Family: Payor ID#80142
- Jefferson Health Plans Medicare PPO: Payor ID#RP099
Connection to SDS is live and ready to receive claim submissions. Providers may sign up through the SDS provider portal by emailing SDS directly at stream.support@sdata.us. Be sure to include the following information: First Name, Last Name, email, phone, Organization name, Organization NPI, Organization Tax ID, and the Payor IDs listed above.
If you have any questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.). Thank you for your kind attention to this important matter.
March 5, 2024 - Ancillary Provider Orientation and Training Announcement
Thank you for being a valued Jefferson Health Plans participating provider. Jefferson Health Plans is hosting our Ancillary Provider Orientation and Training webinar of 2024! The live webinar will be held on Wednesday, March 27, 2024, 12:30 to 1:30 p.m., tailored to the services provided by the provider types below:
- Radiology
- Home Care
- Home Hospice
- Home Infusion
- Transportation
- Home Health Aide
- Ambulatory Surgical Center
- Skilled Nursing Facility (SNF)
- PT, OT and Speech Therapy
- Durable Medical Equipment (DME)
This webinar will provide current and newly credentialed providers with a comprehensive review of our administrative services and processes.
Topics include:
- 2024 updates
- Overview of online tools
- Claim filing instructions and best practices
- Credentialing
- Prior authorizations and Evicore
- Cultural Competency
REGISTRATION DETAILS
As stated above, the webinar will be held on March 27, 2024, from 12:30 – 1:30 p.m. and will include a Q&A session. Webinars are free, but registration is required. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
If you have any questions, call the Provider Services Helpline at 1-888-991-9023 (Monday – Friday, 9:00 a.m. - 5:30 p.m.) or email ProviderCommunications@jeffersonhealthplans.com.
We look forward to your participation and your continued commitment to remain up to date on Jefferson Health Plans practices.
March 5, 2024 - Provider Annual Orientation and Training Webinar Announcement
Jefferson Health Plans is hosting our first provider orientation and training webinar of the year on March 20, 2024. Jefferson Health Plans requires all participating providers to demonstrate that they are knowledgeable and trained on important topics and participate in at least one of four quarterly webinars each year. Participation in this webinar will satisfy this annual requirement.
This webinar will provide current and newly credentialed providers a comprehensive review of Jefferson Health Plans’ benefits, administrative services and processes.
Topics include:
- 2024 updates
- Health Partners (Medicaid), KidzPartners (CHIP), Jefferson Health Plans Medicare and Individual and Families plans
- Lab and other benefit carriers
- Online tools (including provider portal, website, etc.)
- Claim filing instructions and best practices
- Community HealthChoices program
- Maternity services
- Access and availability standards
- Pay-for-Performance and Quality Care Plus
- EPSDT standards
- Special HIV/AIDS services
- Member identification cards
REGISTER TODAY
To register, select the webinar you are interested in attending and click the registration link in the description. You will receive an email that confirms your registration and gives you the option to add the webinar to your calendar.
ALTERNATE OPTION
While participation in this live webinar will satisfy your annual Jefferson Health Plans training requirement, there is an alternative method to complete the training. Please visit our Provider Online Courses page to access the Provider Orientation and Training eLearning course. Simply review with your staff and submit the electronic attestation found at the end of the training.
D-SNP MODEL OF CARE TRAINING
Successful completion of the D-SNP Model of Care training module is mandatory for providers serving Jefferson Health Plans Medicare-Dual Eligible Special Needs Plan (D-SNP) members. At least one member of a care team location is required to take the annual online training course and distribute the training material to all D-SNP care team members.
ACCESS AND APPOINTMENT & AVAILABILITY STANDARDS
Timely access to quality health care is extremely important for our members. As you should be aware, it is a regulatory requirement that all Jefferson Health Plans-participating providers must meet clearly defined access, appointment and availability standards. These standards can be found in Chapter 11: Provider Practice Standards & Guidelines, of the Jefferson Health Plans Provider Manual, available by going to the Provider Manual page.
To help ensure that your site is adhering to appropriate timeframes for scheduling and availability, we have enclosed copies of these standards for PCPs, Specialists and OB/GYNs. These documents include:
- Provider Access and Appointment Standards
- Telephone Availability Standards
JEFFERSON HEALTH PLANS ACCESS AND AVAILABILITY SURVEYS
Each year, Jefferson Health Plans surveys our providers to determine if they are meeting these standards. A new mandatory survey is planned for Q2. We look forward to your participation.
Thank you for your support in providing the highest quality of care to our members.
February 28, 2024 - Spring 2024 Provider Check Up Newsletter is Now Available!
The Spring edition of the Jefferson Health Plans’ provider newsletter, Provider Check Up, is now available on our Provider Newsletters main page.
In this issue, we provide information on the following topics:
- Jefferson Health Plans Product Updates
- KidzPartners (CHIP) Expansion Update
- Data Validation
- 2024 Webinar Series Information
- CAHPS Information
- Member Rewards Updates
- Hepatitis C: Screening and Treatment
- Controlling Hypertension
- Antibiotic Stewardship
- Advance Care Planning
- Preconception Healthcare and Counseling
- Childhood and Adolescent Immunizations
- Pharmacy Formulary Changes
- Tips for Preventing Fraud
- Preclusion Check Information
- Policy Bulletin Updates
- Cultural and Linguistic Requirements and Services
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
February 23, 2024 - Change Healthcare Cyber Security Incident: Authorization Process Update
As recently communicated, on February 21, 2024, Jefferson Health Plans was alerted by Change Healthcare about a cyber security incident they’ve experienced that is disrupting Change Healthcare’s ability to deliver services.
We will continue to monitor this situation and, dependent on the duration and/or severity of the incident, may modify the below interim process changes upon written notice.
FAQs are posted below to answer overall questions; this posting is to clarify questions specifically around our authorization process during this incident.
- Authorization requests should continue be submitted through our provider portal, as that is the most efficient flow of authorization submissions
- We will still require notification of admissions
- Clinical documentation will still be required to be submitted as soon as it is available
- We will still adhere to regulatory timelines in rendering decisions
- Acute inpatient admission requests will be reviewed based on a combination of InterQual guidelines and medical necessity.
- For the Medicaid and CHIP lines of business, we will allow reconsiderations to be submitted at any time during the incident, and for 30 days post outage resolution
- For Medicare, we will continue to utilize the “2 midnight rule” along with NCD/LCD to facilitate medical necessity determinations
- Prior authorization requirements will remain in place following regulatory timeframes and requirements
Thank you for your attention to this matter.
February 22, 2024 - Change Healthcare Outage
On 2/21/24, Jefferson Health Plans was alerted by Change Healthcare about a network outage that is disrupting Change Healthcare’s ability to deliver services. This impacts providers who use Change Healthcare to send member eligibility verifications, 837 files and paper-to-electronic claims scanning. In addition, it impacts InterQual service that we use to determine appropriate levels of care and may cause delays in determinations.
Updates to this outage can be found on Change Healthcare's status site here: Optum Solutions Status. Jefferson Health Plans will continue to provide updates as they are received.
Update: Some applications are experiencing connectivity issues.
Optum Solutions's Status Page Update: Some applications are experiencing connectivity issues.
Providers who receive paper checks will experience delays in payment. Checks will not be printed until this incident is resolved. Electronic payments are not affected.
Click here for for more information on how to receive electronic payments/remittances.
February 16, 2024 - Women's Health Measures and Maternity Quality Care Plus (MQCP)
You’re invited to participate in an upcoming webinar on women’s healthcare topics on Wednesday, February 28, 2024. This webinar will review important details related to Jefferson Health Plans’ programs tied to women's healthcare, offer information about women's health measures, and will provide a first look at a new initiative related to hypertension self-monitoring.
The webinar will cover topics including:
- Maternity Quality Care Plus (MCQP) program
- Obstetrical Needs Assessment Form (ONAF) program
- Baby Partners Program
- HEDIS Measures and Pennsylvania External Quality Review (EQR) measures:
- Breast Cancer Screening (BCS)
- Cervical Cancer Screening (CCS)
- Chlamydia Screening (CHL)
- Prenatal and Postpartum Care (PPC)
- Perinatal Smoke Screening- EQR (PSS)
- Prenatal Depression Screening- EQR (PDS)
- Overview of an upcoming initiative: Hypertension self-monitoring with digital blood pressure cuffs for pregnant members
REGISTRATION DETAILS
This 45-minute webinar will be held on Wednesday, February 28 at 12:00 p.m. and will include a Q&A session. Webinars are free, but registration is required.
If you have any questions, call the Provider Services Helpline at 1-888-991-9023 (Monday–Friday, 9:00 a.m. to 5:30 p.m.) or email ProviderEducation@jeffersonhealthplans.com.
Thank you for your support in providing the highest quality of care for our members.
February 15, 2024 - PCMH Specialist 7-Day Follow-Up
As a requirement of the DHS Patient-Centered Medical Home (PCMH) program, patients admitted with an ambulatory sensitive condition must be seen by the primary care PCMH provider or specialist provider within seven days of discharge from the hospital. If the follow-up appointment takes place with a specialist, the specialist provider must share the patient’s follow-up visit notes with the primary care PCMH provider to meet this requirement.
February 5, 2024 - 2024 Medicare Member Wellness Rewards
Jefferson Health Plans will continue to offer Wellness Rewards, our Medicare rewards program, to all Medicare members in 2024. Wellness Rewards incentivizes Medicare members to complete specific health-related activities to earn rewards dollars on a reloadable flexible spending card. Please note that our Medicare rewards program is different from our Medicaid/CHIP rewards program.
January 31, 2024 - MQCP Manual
Thank you for being a Jefferson Health Plans participating provider and for your continued participation in our Maternity Quality Care Plus (MQCP) program. MQCP is designed to recognize and reward your practice’s performance in delivering high-quality services throughout the year. Every year, we assess the program to ensure a positive impact on both our members and our provider network.
The 2024 MQCP Manual is now available on the provider portal and here. Please note that the manual will not be mailed to your office.
In October 2023, we shared updates to the 2024 MQCP program with our provider network. Details of those updates can be found in this manual.
As a reminder, ONAF has been removed as an MQCP program measure and is now a separate reimbursement program.
Your Provider Relations Representative will work closely with you to answer any questions and ensure that your office understands all 2024 changes. Thank you for your support in providing the highest quality of care to our members.
January 30, 2024 - 2024 Individuals and Families Resources
We are pleased to announce the live recording and presentation for the 2024 Individuals and Families OEP webinars held in October 2023 are now published to the provider page of our website, in addition to a self-led eLearning course.
As a reminder, the webinar and eLearning course offers a detailed overview of the benefits in our plans, including:
- Plans in Bronze, Silver, and Gold tiers available both on and off exchange
- Low premium, affordable plans (lowest premium Silver plan)
- $0 Medical deductible plans available in all tiers
- Free first PCP visit on all plans
- No referral requirements
Please visit our Provider Online Courses for access to provider online courses.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
January 30, 2024 - Blood Pressure Cuff Guidelines
Effective immediately, we have simplified ordering a blood pressure cuff for our Medicare, Medicaid, CHIP* and Individual and Families (Exchange) lines of business.
We encourage you to provide guidance to your patients on the proper use of the blood pressure cuff along with how often to take a blood pressure reading and report the results to your office. Please instruct your patients to bring their blood pressure equipment with them to their next appointment so your staff can check for correct usage.
To order a blood pressure cuff for a member:
- Members must be 18 years of age or older OR pregnant.*
- Use the blood pressure cuff form that is located on our Form and Supply Requests page.
- Complete all sections to ensure prompt, accurate shipping.
- Email or fax the completed form following the directions on the bottom of the form.
If you have any questions, please contact our Provider Services Helpline at 1-888-991-9023 (Monday-Friday, 9:00 a.m. to 5:30 p.m.).
January 29, 2024 - Jefferson Health Plans 2024 Medicare & Individuals and Families Webinar
You're invited to an upcoming Jefferson Health Plans’ Medicare/Individuals and Families (IFP) webinar. Our team will provide a review of the Medicare Advantage and IFP products and other guidelines, including:
- Medicare Advantage products for 2024
- Individuals and Families Plans for 2024
- Provider Portal
- Claims
- Utilization Management and Prior Authorizations
- Evicore
- Contact & Resources
REGISTRATION DETAILS
The webinar will be held on Wednesday, February 14, 2024. Providers are encouraged to attend this session to learn more about these topics. The webinars are free, but registration is required.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
Thank you for your partnership in serving our members.
January 18, 2024 - Pennsylvania Statewide Preferred Drug List - Asthma Inhaler Coverage
GlaxoSmithKline (GSK) has discontinued manufacturing Flovent HFA and Diskus as of December 31, 2023.
For our Medicaid members, we will cover Flovent HFA and Diskus until supplies are no longer available. Once supplies are depleted, patients will need to be switched to a preferred alternative. Please note, generic Fluticasone Propionate HFA and Fluticasone Propionate Diskus are non-preferred on the Statewide PDL.
Below is a list of the preferred drug list alternatives.
Preferred Alternatives:
- Arnuity Ellipta
- Asmanex HFA
- Asmanex Twisthaler
- Budesonide 0.25 mg/2 ml, 0.5 mg/2 ml
- Pulmicort Respule
- Pulmicort Flexhaler
- Qvar Redihaler
- Arnuity Ellipta
For the most up-to-date information, please visit our online formulary. For more information, call our Pharmacy department at 215-991-4300 or our Provider Services Helpline at 1-888-991-9023 (Monday to Friday, 9 a.m. to 5:30 p.m.).
Thank you for your cooperation in improving the quality of care you deliver to your patients and our members.
January 16, 2024 - Maternal Transthoracic Echocardiograms
Effective February 1, 2024, prior authorization for Maternal Transthoracic Echocardiograms (CPT 93306) will no longer be required when accompanied by a pregnancy diagnosis (O09.00-O9A.53).
Transthoracic Echocardiograms without a pregnancy diagnosis will still require prior authorization, following the standard process through eviCore.
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday - Friday, 9 a.m. to 5:30 p.m.).
January 16, 2024 - Expansion of CHIP Program Offering
We are excited to announce that we are expanding our Children’s Health Insurance Program (CHIP). It is now offered in all 67 counties across the Commonwealth of Pennsylvania.
We bring a wealth of experience partnering with providers to effectively coordinate and manage the healthcare needs of children. We take great pride in the relationships we develop and nurture with our provider partners.
We look forward to working collaboratively with you and the other providers in our network to meet the needs of our members and assuring they receive the highest quality of care.
For reference, a sample ID card is provided below:
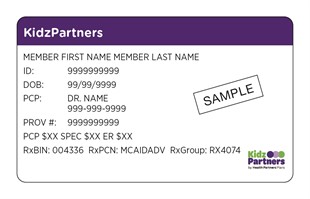
If you have any questions, please call the Provider Services Helpline at 1-888-991-9023 (Monday–Friday, 9 a.m. to 5:30 p.m.)
January 5, 2024 - Billing/Regulatory Guidance for Hospice Providers
In preparation for upcoming provider monitoring that Jefferson Health Plans’ Special Investigation Unit will be performing, we would like to make you aware of some recent findings of Pennsylvania Department of Human Services (DHS) medical records reviews for Hospice providers.
Below is a summary of those findings and applicable regulatory guidance to assist in ensuring the highest level of accuracy in the documentation of Hospice services.
- The patient’s medical record should include sufficient documentation related to the patient's terminal illness, including an applicable terminal illness form. Please refer to[55 Pa. Code§ 1101.51 (e)(1 )(x); and § 1130.22(1 )(ii)(2)(i)(ii)(B). See also 55 Pa. Code§§ 1130.21 (3), and 1130.91.] for more information.
- Medical records should always include notice of rights and responsibilities. [55 Pa. Code §§ 1130.52(a)(1)(3)(4)(5)(b) and 1130.61 (3).]
- Medical record must be legible, accurate, complete and chronologically reflect the evaluation and treatment of the recipient. [55 Pa. Code Chapters 1101, 1130, and all applicable MA Bulletins.]
- Medical record should include sufficient documentation of social worker visits and bereavement counseling notes, as specified in the plan of care. [55 Pa. Code§§ 1130.52(a)(1)(b), 1130.61(4) and 1130.62(2) and (4).
- Oral certification of terminal illness was not followed up with a written certification in a timely manner.[55 Pa. Code § 1101.51(e)(1)(x); and 55 Pa. Code § 1130.22(1)(2). See also 55 Pa. Code § § 1130.21(3) and 1130.91.]
- Terminal illness form should be reviewed and recertified in a timely manner. [Please refer to 55 Pa. Code§ 1101.51 (e)(1 )(x); and § 1130.22(1 )(ii)(2)(i)(ii)(B). See also 55 Pa. Code§§ 1130.21 (3), and 1130.91. for more information.]
- Medical record was missing the initial Certification of Terminal Illness form [in violation of 55 Pa. Code § 1101.51 (e) (1)(x); and 55 Pa. Code § 1130.22(1)(2)(5). See also 55 Pa. Code §§ 1130.21(3). 1130.71©, and 1130.91].
- Medical record had an untimely/missing Recertification of Terminal Illness form. The hospice must obtain written Recertification of Terminal Illness with two calendar days after beginning of each 60-day benefit period occurring subsequent to the initial 60-day period during which the recipient was admitted to hospice [in violation of 55 Pa. Code § 1101.51 (e)(1)(x); and 55 Pa. Code § 1130.22(3). See also 55 Pa. Code §§ 1130.21 (3) and 1130.91].
- Hospice related services or medications should not be supplied by another provider while the member is enrolled in hospice. [Please refer to 55 Pa. Code §§ 1130.52 (a)(1)(b), 1130.61(1)(4), and 1130.62 (8). See also 55 Pa. Code § 1130.91 and MA Bulletin 37-02-01 for more information.]
- Codes G0155 and G0299 were submitted as a claim with dates of services provided outside of the last 7 days of the recipient’s life. Please refer to [55 Pa. Code § 1101.75(a)(4)(6)(8). See MA Bulletin 06-15-02, effective date January 1, 2016. See also 55 Pa. Code § 1130.91].
If you have any questions, please contact the Provider Services Helpline at 1-888-991-9023 from Monday-Friday 9:00a.m. to 5:30p.m.
January 5, 2024 - Policy Notification: Professional Telehealth Services (Individual & Family Plans)
Effective January 1, 2024, Jefferson Health Plans will be implementing a new claim payment policy: RB.038.A Professional Telehealth Services (Individual & Family Plans).
You can access this policy by visiting our policy bulletin library.
As a reminder, our medical policy bulletins define medical necessity criteria and coverage positions on topics such as medical services, procedures, DME, therapies, etc., while our claim payment policy bulletins provide reimbursement rules and billing guidelines necessary to ensure timely and appropriate payment.
News Archive
For news and updates prior to 2024, please email providereducation@jeffersonhealthplans.com.
Additional Resources
Published quarterly, the Jefferson Health Plans provider newsletter includes important updates for our network. Each issue contains health education news, updates to policies and procedures, training and education opportunities, member benefit information and more.
Effective April 1, 2023, continuous enrollment for Medical Assistance and CHIP has ended. There is potential impact to your practice and to your patients if they do not submit their annual renewal application on time.
Please call our Provider Services Helpline at 1-888-991-9023 (9:00 a.m. to 5:30 p.m., Monday-Friday).